Introduction
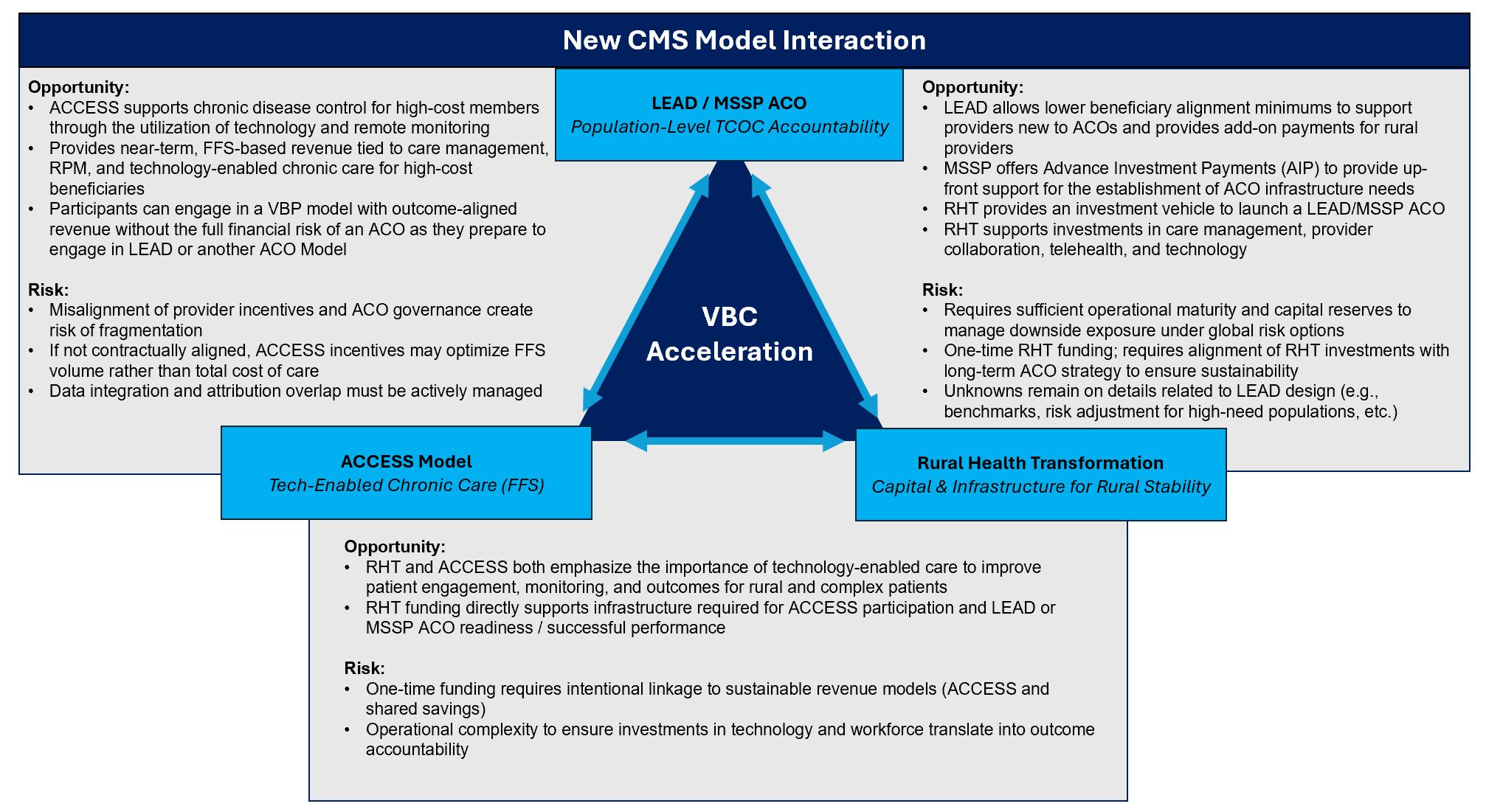
Over the last 30 days, CMS and other federal agencies released several major policy and payment model announcements, many of which landed quietly over the holidays. While numerous regulatory updates were issued, three developments stand out as especially consequential for providers nationwide:
- Announcement of the LEAD ACO Model
- Announcement of the ACCESS Model (Medicare FFS)
- Awards made to states for the Rural Health Transformation (RHT) Program
Collectively, these recent developments emphasize four common themes that should guide strategic priorities for providers:
- Reducing total cost of care
- Strengthening quality and payment for outcomes
- Improving care coordination and member engagement
- Leveraging technology and data analytics
With the announcement of these CMMI program updates, the next 6-12 months represent a critical inflection point in building a coherent value-based strategy and infrastructure – particularly for FQHCs, physician groups, rural hospitals, existing ACOs, and other organizations considering a new alternative payment model. This article highlights key synergies across these programs, along with practical considerations for providers seeking to begin planning to capitalize on available funding, strengthen financial sustainability, and improve patient outcomes in 2026, 2027, and beyond.
LEAD ACO Model: The Next Evolution of Accountable Care
Beginning in January 2027, the LEAD Model (Long-term Enhanced ACO Design) is a successor to ACO REACH which implements lessons learned from other current and prior ACO models. LEAD continues CMS’s focus on primary care-led models, but with greater focus on increasing the scope of ACOs (e.g., including more small, rural, and/or independent providers) and enhancing care coordination for high-needs patients, with a long-term vision of closer Medicare-Medicaid integration to improve outcomes for dual-eligible beneficiaries.
While LEAD will carry forward some familiar design elements from prior models (e.g., prospective payments, professional/global risk tracks), several newer features stand out, including:
- A 10-year performance period with no benchmark rebasing, providing stability for providers to make greater investment in capabilities and technology with longer-term returns.
- New Benefit Enhancements and Beneficiary Engagement Incentives to encourage members to seek care from ACO providers (i.e., Part B cost sharing, Part D premium buy-down, medical nutrition therapy).
- Greater support for rural providers, including add-on payments as well as lower beneficiary alignment minimums for ACOs with providers new to ACOs.
- Integration of support for high-needs patients, including more accurate risk adjustment and benchmarking, to incentivize providers to develop capabilities to care for patients with complex needs.
For organizations already participating in – or considering entry into – Medicare ACO models, LEAD represents a potential pathway into a more stable, long-term accountable care framework, with a longer runway for multi-year investments in care management, analytics, and provider engagement.
- For existing ACOs, organizations should map attributed panels, current performance, and infrastructure against LEAD expectations to evaluate how to approach a transition into LEAD.
- Providers considering first-time ACO participation (i.e., FQHCs, physician groups) should run a financial analysis against VRDC Medicare data and assess their data and performance management capabilities, risk tolerance, and the required governance structure to determine best fit for ACO participation1.
ACCESS Model: Reimagining Medicare FFS with Technology-Enabled Chronic Care
Launching in July of 2026, the ACCESS Model (Advancing Chronic Care with Effective, Scalable Solutions) is a 10-year voluntary, outcome-aligned payment model in Original Medicare, with the stated aim of testing whether expanding technology-enabled care can reduce total Medicare spending while improving chronic disease management. Organizations interested in participating in ACCESS must be enrolled in Medicare Part B – Medicare Advantage organizations may not participate in the ACCESS model directly under current eligibility rules.
ACCESS Payment Approach:
- Rewarding Results: Under ACCESS, participating organizations receive recurring outcome-aligned payments (OAPs) for the management of qualifying chronic conditions, with additional payment tied to the achievement of specific outcomes reflecting clinical improvement or control of a patient’s condition (A1C, blood pressure, weight, lipid control, pain scores, or validated behavioral health measures). Failure to achieve outcomes can reduce or eliminate some portions of OAPs.
- Integrated Co-Management: To support integration with primary care and referring clinicians, ACCESS allows clinicians who co-manage beneficiaries with an ACCESS participant to bill a new co-management payment (~$30 per service, up to ~$100 per beneficiary per year) for documented review of ACCESS updates and related coordination activities.
This program relies on API-based data exchange, including eligibility and alignment APIs, the Beneficiary Claims Data API for optional claims feeds to support coordination of care. It is also flexible in allowing virtual, in-person and asynchronous care plus FDA authorized devices/software in the care model.
Current eligibility criteria risk potential misalignment of provider incentives and managing TCOC. While we anticipate some adjustment to eligibility and other aspects of ACCESS as CMS continues to engage with stakeholders, the overall model of payment tied to technology-driven outcomes is expected to remain a key aspect of ACCESS and migrate into other models over time, including Medicare Advantage, Medicaid managed care and commercial lines of business.
Rural Health Transformation: Accelerating Value-Based Care for Rural Providers
Recognizing that traditional fee-for-service has failed to sustain many rural hospitals and providers, the Rural Health Transformation (RHT) Program signals a renewed federal focus on stabilizing rural providers and accelerating their participation in value-based care with a commitment of $50 billion over 5 years. Beyond the scale of the investment, RHT showcases CMS’ willingness to offer new pathways, flexibilities, and potential upfront support to bring rural providers into alternative payment models.
The RHT program creates distinct opportunities across provider types:
- Rural Providers: Assess the operational and data capabilities required to succeed in VBC to align capital/IT plans (e.g., telehealth, RPM, data analytics) with RHT priorities. Leverage RHT as a bridge into sustainable participation in ACOs and other value-based arrangements rather than relying solely on FFS.
- Health Systems and ACOs: Evaluate rural footprint and consider how RHT investments can support attribution growth, care management, and post-acute networks in rural markets. ACOs should evaluate how state-level RHT initiatives align with your benchmarks, TCOC targets, and appetite for risk.
- FQHCs & Physician Groups: Consider how you can partner with rural hospitals or regional systems in clinically integrated networks and hub-and-spoke models to improve efficiency, access, and outcomes.
All 50 states were awarded RHT funding, with first-year funding in 2026 ranging from $147M to $281M. Accordingly, CMS published each state’s RHT Project Abstract outlining how each state intends to deploy funds. As states begin to execute on these plans, providers must closely monitor local priorities and funding allocation to guide ongoing strategy and decision-making.
Bottom Line
Across LEAD, ACCESS and RHT, federal policy is clearly signaling four interconnected priorities: lowering total cost of care, improving quality, strengthening member engagement and care coordination, and accelerating technology-enabled care.
While key details and potential changes for these models remain, many of the underlying model concepts (i.e., technology-enabled care and outcome-based payment) will become the new norm for Medicare FFS, and will likely begin to appear across Medicare Advantage and other managed care lines of business.
For providers, the strategic questions heading into 2026–2027 are becoming less about whether to participate in value-based care, and more about which models best fit their population, capabilities, and risk tolerance. Success will depend on aligning strategy with long-term sustainability rather than short-term incentives, and on building (or partnering) for the infrastructure required to manage total cost of care across multiple programs and populations.
For more information and to talk through your organization’s next move, reach out to us at info@copehealthsolutions.com or visit us at copehealthsolutions.com.
Footnotes:
1 For more comprehensive information on the LEAD model and how CHS can help you succeed as a Medicare ACO, see our prior article linked here.