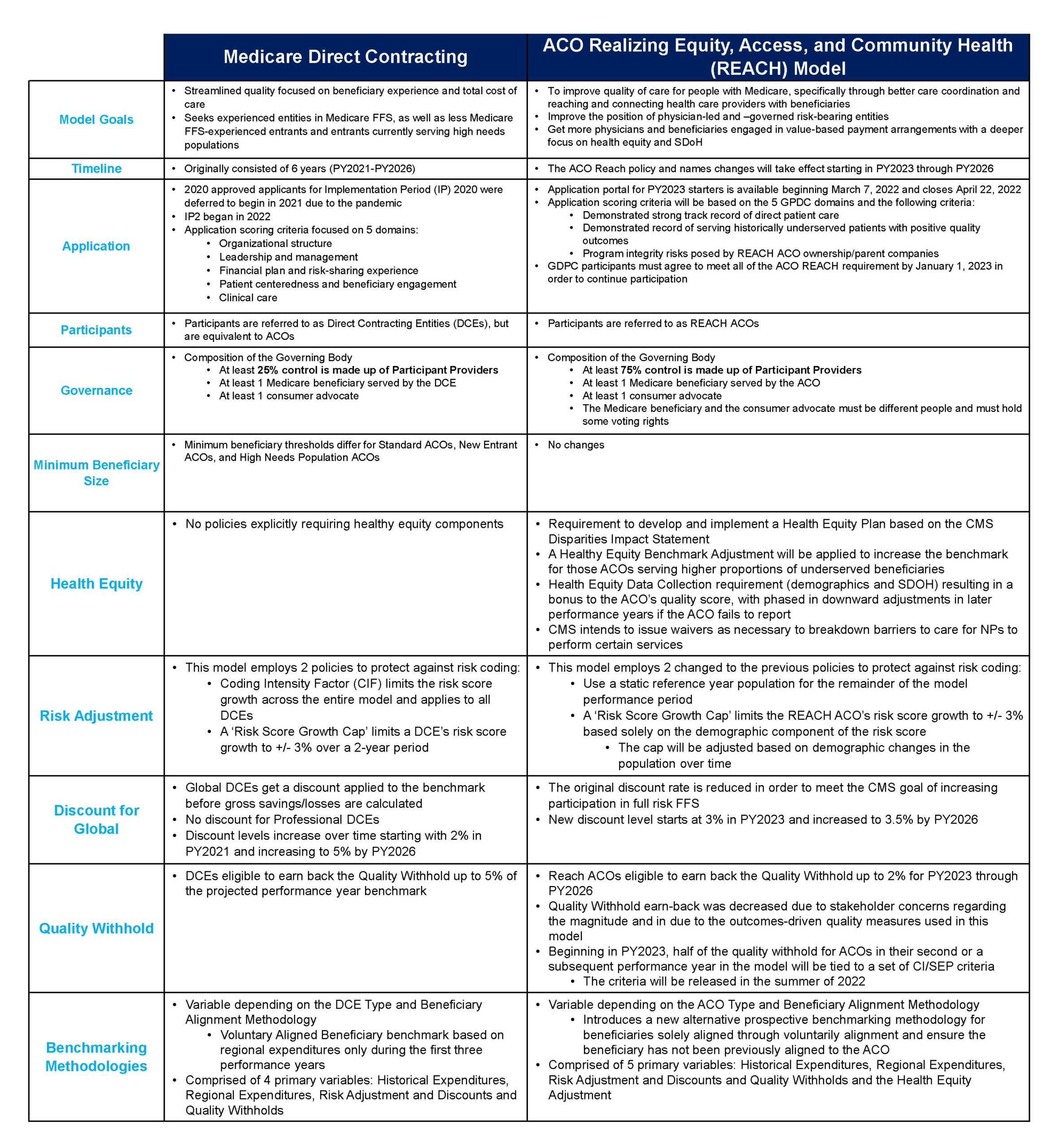
Health care providers have a narrow window to decide to take advantage of the newest alternative payments program from the Center for Medicare and Medicaid Innovation (CMMI). Just two weeks ago, CMMI announced it is replacing the Medicare Direct Contracting program with the ACO Realizing Equity, Access, and Community Health (ACO REACH), an accountable care organization model with an increased focus on care disparities and social determinants of health (SDoH).
- The April 22 ACO REACH application deadline is looming.
- Indications are ACO REACH applications will not reopen until this first round of the demonstration project concludes in 2026.
Why apply for ACO REACH?
1. ACO REACH offers an important opportunity for providers to gain competency and build capabilities as they bridge to value-based care and payments:
- Align financial incentives for managed care and fee-for-service (FFS) populations
- Obtain data for FFS and managed care populations
- Incorporate SDoH and health equity initiatives
2. As with MDC, there are two risk levels so providers can choose the one that better suits their level of experience with population health and cost management. The Professional Risk capitation option limits the downside exposure while the Global Risk capitation model offers more upside potential as well as downside risk.
3. With MDC phasing out, Direct Contracting Entities (DCEs) that want to continue with a CMS program offering professional or global risk will not need to apply for ACO REACH. However they will need to explain how they will meet the new program criteria, including addressing SDoH and health equity and a ACO board comprised of 75% physicians vs. 25% for MDC by January 1, 2023.
4. Providers can apply and then choose to retract their applications later with no penalty.
For help with assessing your fit with ACO REACH or your application, contact us at info@copy.laraco.net.

