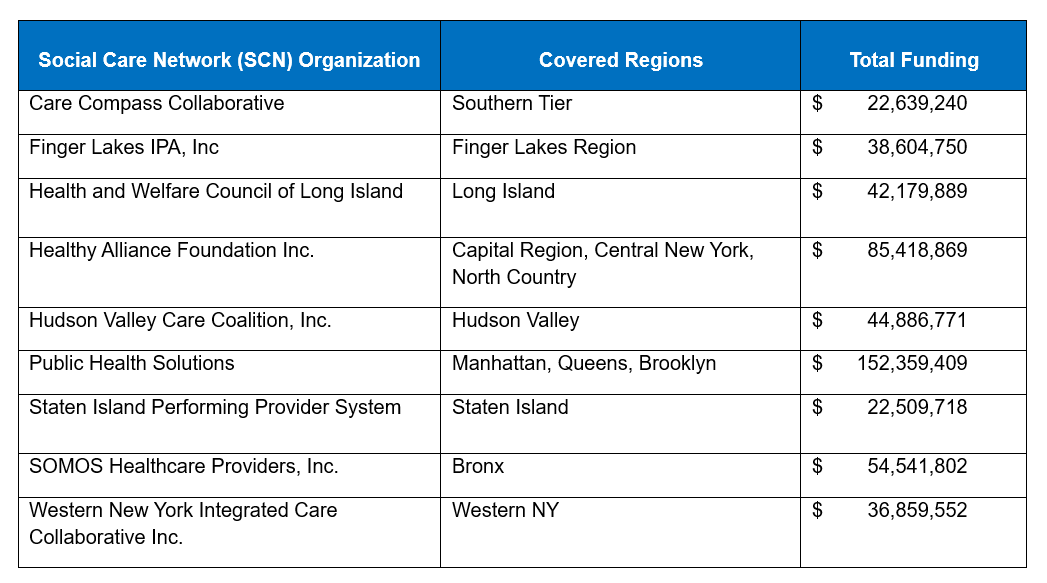
New York State has revealed the nine organizations awarded with Social Care Network (SCN) status under the 1115 Medicaid Waiver Amendment. One of the state’s main goals under the 1115 Waiver is to invest in the screening and delivery of Health-Related Social Needs (HRSN) services to reduce health disparities and improve quality outcomes. SCNs will be the crucial entities tasked with building networks of contracted community-based organizations (CBOs), while also engaging providers, Medicaid Managed Care Organizations (MCO), and other stakeholders, to create a strong social care service delivery system.
A total of $500 million will be available as infrastructure funding to stand up SCNs.
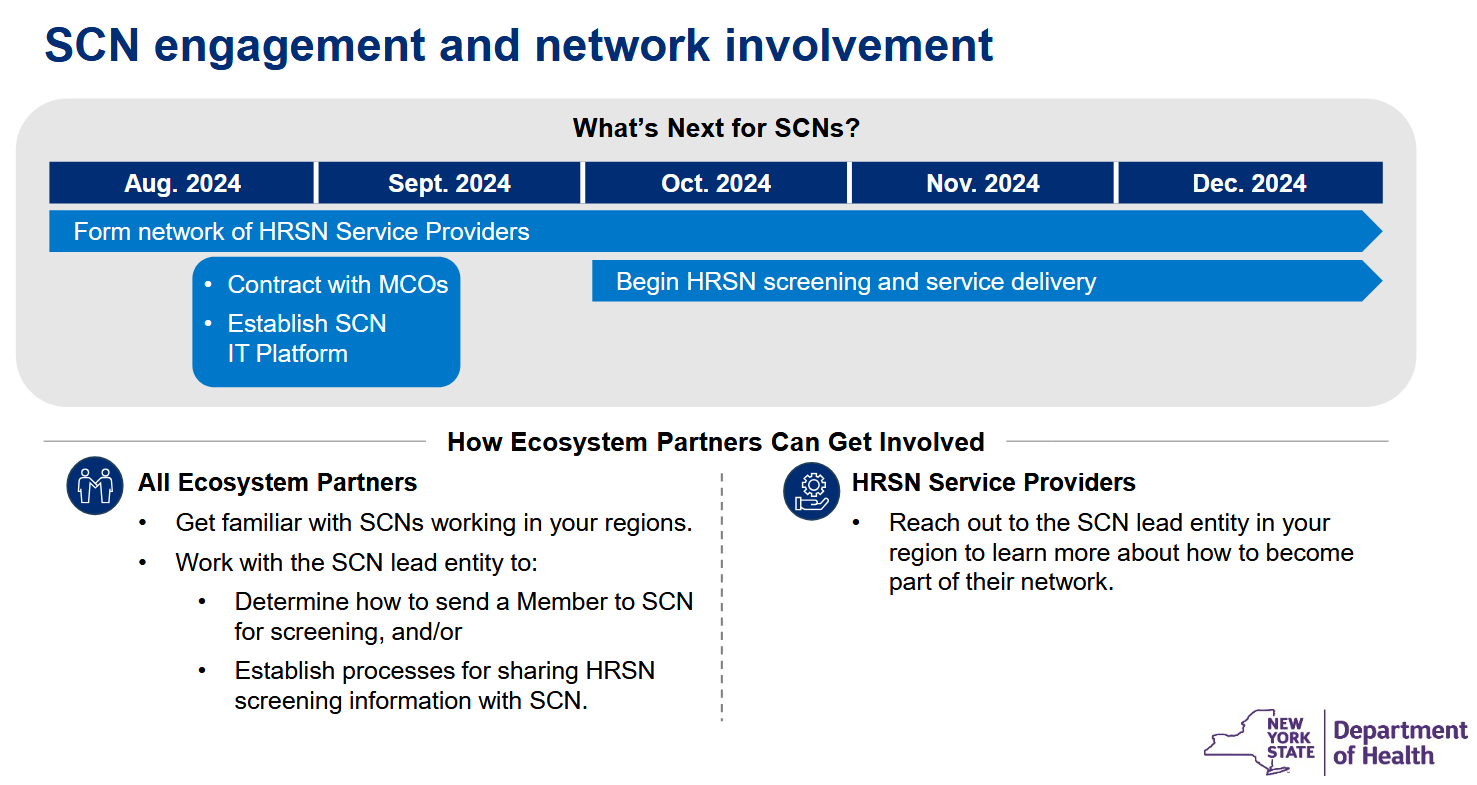
Amir Bassiri, New York’s Medicaid director, presented the updated timeline below in United Hospital Fund’s annual Medicaid conference last week.
Key Actions for SCNS to Take Right Now
Key Actions for Provider Groups (IPA, CIN, ACO)
Key Actions for MCOs
Key Actions for SCNS to Take Right Now
- Evaluate CBO partners in the region that will deliver HRSN services. While you may have already identified local CBOs and gathered LOIs to participate in your network, a crucial next step is to assess each CBO’s operational capacity in order to build an adequate and optimal CBO network to meet demand for HRSN services. To do so, your SCN will need to evaluate each CBO’s current HRSN service mix, staffing, and infrastructure and determine whether the CBO is a good fit for your network, and, if so, the appropriate level of investment needed to build capacity. SCNs can invest in CBOs through purchasing equipment, providing training or technical assistance, or hiring additional resources.
- Establish partnerships with key stakeholders to provide screening and service navigation to HRSN services for eligible Medicaid members. These stakeholders include MCOs, providers, care management providers, health homes, and behavioral health providers. They are critical for engaging Medicaid members, certifying eligibility for HRSN services, and closing referral loops. Engagement of MCOs is particularly critical to establish structures necessary to reimburse CBOs that deliver social care services.
- Establish an SCN governing body with the correct makeup of representatives and executive leadership team that monitors day-to-day operations. It will be critical to develop a clear roadmap to develop the necessary operational and business practices, including finance and accounting, human resources, and vendor management. SCNs should consider forming standing operational committees for network development, quality, finance, partnerships and strategic initiatives, and other key functions.
- Enhance technology systems by selecting the right vendor(s) and beginning implementation of the “data and IT platform” that will enable social care data sharing and interoperability between SCNs, CBOs, other stakeholders, and NYS through the Statewide Health Information Network for New York (SHIN-NY). Minimum product requirements of the data and IT platform should include: member information, screening, referral and service delivery, payment and fiscal administration, performance management, compliance and user access, and data sharing and exchange.
- Establish quality improvement programs to enhance service delivery and outcomes. Design programs to assess and improve care processes, patient experiences, and health outcomes. Key elements include setting clear quality goals, developing data-driven metrics for evaluation, and implementing evidence-based interventions to address identified gaps.
CHS can help with your first steps as you assess your CBO network and begin to outline a framework for distribution of capacity-building funds and technical assistance.
- CBO Capacity and Infrastructure Funding Tool is built to assess capabilities of each CBO, inform decision support for distribution of capacity-building funds and identify gaps where training or support services from the SCN or its partners will be needed across the CBO network. The tool is designed to help SCNs meet reporting requirements for utilization of funds, assess and build a high-performing network that will enable them to achieve bonus payments available in Year 2 and 3 of the waiver, and establish a value proposition to MCOs for long-term sustainability of the SCN after the waiver.
- Consulting services for technical assistance to the SCN or partner CBOs for IT vendor assessments and implementation support, data capture and analytics, MCO contracting, financial modeling, member stratification and outreach, workflow design and implementation, provider communication and engagement strategies, care model design, workforce development, care team structure and training, HEDIS quality and HRSN gap closure, and patient outreach and engagement.
Key Actions for Provider Groups (IPA, CIN, ACO)
- Align shared goals and strategies with the regional SCN to integrate social care into clinical care plans for Medicaid beneficiaries to ensure a holistic approach to patient care. Look for win-win opportunities to partner with the SCN to help manage and reduce cost of care for any of your attributed members.
- Evaluate whether your organization can access the SCN’s chosen data and IT platform in order to participate in HRSN screening and service navigation, including certifying member eligibility for HRSN services. This connection will also enable the sharing of patient data between IPAs/CINs/ACOs and SCNs. Investing in interoperable IT systems is essential to maintaining compliance and facilitating data exchange and communication across networks.
- Implement the NYS-standardized HRSN screening tool, adapted from the Accountable Health Communities (AHC) screening tool, in clinical and non-clinical settings to identify patient eligibility and HRSNs. Once identified, a streamlined referral process can connect patients with the appropriate HRSN services, either through connecting patients to the SCN or directly to CBOs if the organization has access to the data and IT platform.
- Provide training for clinical and administrative staff on the importance of addressing HRSNs and utilizing SCN resources. Training will ensure that all team members understand the impact of social factors on health outcomes.
- Review outcomes and processes to identify areas for improvement to enhance care coordination and patient outcomes. Collect and analyze data on patient outcomes, service utilization, and care processes to gain insights on quality improvement opportunities.
CHS can support your organization to assess its readiness to engage with the regional SCN and develop value-based care capabilities to succeed in broader risk arrangements.
- ARC platform provides a complete VBP management solution integrating claims data, EMR data, HRSN screening and CBO services data, and care management data for:
- Assessment of intervention effectiveness and quality improvement through performance reporting and advanced analytics
- Seamless HRSN data sharing, real-time care coordination, and comprehensive reporting in conjunction with SCN data and IT platform
- Closed loop referral integration with performance reporting and financial modeling
- Coordinated care dashboards to analyze data to understand underlying issues, facilitating better integration of social care into clinical care plans
- Data integration, real-time care coordination, and comprehensive reporting to demonstrate the impact of care initiatives, aiding in continuous improvement efforts
- Consulting services to support strategic & operational alignment with SCNs and joint approaches to maximize payer contract performance across all LOBs and programs, including MSSP ACO, ACO REACH, AHEAD, and Making Care Primary
- Consulting services to integrate CBOs and HRSN services into the broader care model to create a right care, right place, right time network and improve quality, documentation, and total cost of care
Key Actions for MCOs
- Contract with SCNs for PMPM payments to cover HRSN screening and approved Enhanced HRSN services for eligible members. Most SCN entities will be new to the contracting process and may lean heavily on you for guidance and technical assistance to complete contracting.
- Align on IT, data and interoperability solutions to prepare for processing of new HRSN claims, sharing of HRSN screening and referral data, and reporting to NYS on performance of the SCNs and ROI of HRSN services. Identify a vendor or build capabilities to evaluate SCN and CBO performance and ROI including improvement of total cost of care, quality and patient engagement to better understand how HRSN services impact TCOC and plan for changes to premium rates after the waiver.
- Guide network development and capability assessments to advise SCNs on network configuration requirements, CBO performance standards and technical assistance needed. HRSN services are likely to be rolled into risk-based capitation rates after the waiver and MCOs will benefit from using the waiver period to help build out high-performing CBO networks through the SCNs. Look for opportunities to collaborate with SCNs to develop training programs for CBO staff conducting member outreach and screening to cross-train them to focus on identifying and closing quality care gap opportunities and enrollment in disease management or care management programs to leverage this engagement network to further improve cost and quality of care.
- Define data inputs for eligibility criteria and implement workflows to share member lists with SCNs to simplify the eligibility and outreach process. Qualifying criteria for Level 2 services includes defining “high utilizers” and including data elements not typically seen on basic eligibility files (homeless status, health home enrollment, criminal justice involvement) that your technical team will need to prepare and include in eligibility reports for SCNs.
- Establish Joint Operating Committees with each SCN to leverage data, reporting and collaborative decision making to improve outcomes in much the same way as a JOC is used for IPA relationships.
CHS can support your organization to guide development of high-performing CBO networks with each SCN and leverage HRSN services to improve total cost of care and quality.
- ARC platform provides a comprehensive health plan analytics solution including integration of medical and HRSN claims data:
- Full integration with any closed loop referral platform used by SCNs to provide seamless data and reporting on HRSN services utilization and impact on total cost of care
- Robust suite of dashboards to manage performance of the entire network, eligible populations, and individual CBOs or medical providers to optimize performance and service delivery
- Simple financial modeling to easily track and report on ROI of specific funding initiatives and comparison of outcomes across HRSN service types and providers
- Risk stratified chase lists for CBO, SCN or other member outreach partners synthesizing quality gaps, HCC gaps, cost of care opportunities, HRSN screening and service gaps and CM program eligibility
- Network performance for SCNs and CBOs to inform long term network performance optimization
- Consulting services to support strategic & operational alignment with SCNs and joint approaches to maximize total network performance and long-term planning
Contact info@copehealthsolutions.com or 213-259-0245 to see how we can help your organization succeed under the NYS 1115 Waiver amendment.