Part II: Leveraging Financial Incentives and Contracting Strategy
In Part I of this series, we introduced various models in establishing care management organizations within risk bearing entities (RBE), ranging from fully decentralized to fully centralized model. Within these models, three levers influence care management tactics to varying degrees: financial incentives and contract design, organizational and governance structure, and overall operational alignment. Governance organizes the stakeholders to facilitate decision making; however is limited in capturing value without the ability to design and implement the financial arrangements and clinical operations of the network. This article, the second of a three part series, will focus on financial incentives and contracting as tools in driving alignment across the network to manage quality and total cost of care.
You Get What You Pay For
Even in the most mission-driven organizations, business activities are managed to maintain a sustainable margin. In this regard, financial incentives are influential, even if not the dominant force in an organization. It follows then that financial incentives are most impactful when aligned with mission and social good. For this reason, when well designed, value based incentives can motivate and align behavior.
Financial incentives fuel a care management program and are a tool to drive performance in all models of care. The more centralized the model, the easier it is to align incentives. For models that manage care across a decentralized network of providers, the financial incentives are at times the only influence the RBE has over the provision of care and priorities of downstream provider organizations.
Upstream and Downstream Contract Alignment
Contracts between RBEs and providers formalize the commitments made to deliver on value. When an organization takes on risk, it is placing a bet on itself: The odds of winning on shared savings and risk arrangements is directly related to how well aligned care delivery and network performance is with the targets and tradeoffs to which the RBE is contractually committed. To be successful, the RBE must understand the capabilities of the network and ensure that provider payments are adequate to incentivize the activities required to capture adequate value. Organizational priorities must be defined and network capabilities understood so that the RBE can commit to feasible targets and align risk where confidence exists in ability to perform.
When contracting upstream, for example with multiple Managed Care Organizations, aligning the targets and contract terms can help to enable focus on clearer priorities. When contracting downstream, the RBE needs to consult clinical stakeholders and understand the existing care models to, at minimum, remove misaligned incentives and at best add synergistic incentives. Well-designed provider contracts can impact avoidable utilization, site of care optimization, network leakage, and continuity of care.
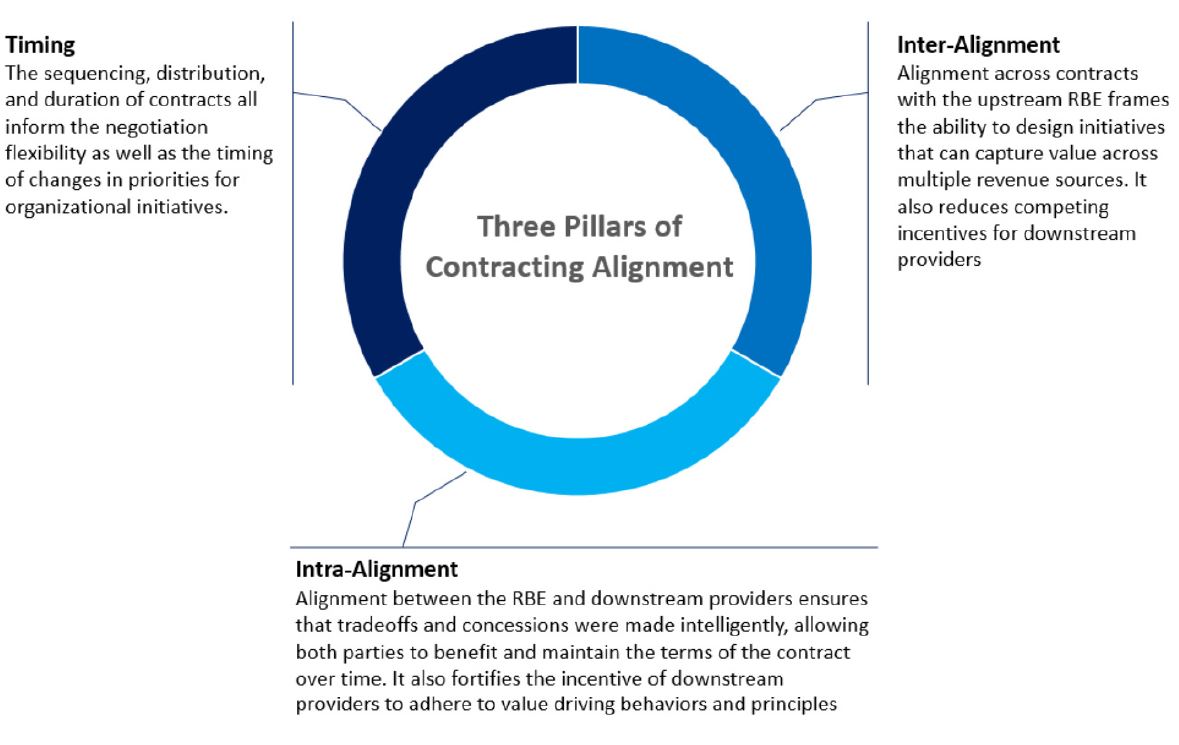
Figure 1: Three Pillars of Contracting Alignment
Redistributing Investment and Reward
The highest cost members have complex needs. To manage these members, RBEs need to ensure the right care is provided at the right time, right place and right intensity. The goal may be to impact a downstream outcome that impacts cost or quality in another care setting. Particularly on decentralized models, the ability to deliberately establish financial arrangements that allow for those who make investments to also reap the reward requires a holistic network level approach in contract design.
Full coordination within a network demands that partners make administrative and clinical investments. Whether data collection, dedicated case conferencing time, or follow ups, providers are embracing what would be opportunity cost under traditional fee-for-service (FFS) environments. It is paramount that the financial context within which they operate supports these activities. For high performing providers, sharing risk can allow them to reap the fruit of their labor, particularly if the reward is based on collective success. There are several contracting deal points that allow parties to conduct this distribution while keeping a fine point on the incentives. Each contract component serves as the financial lever that RBEs can use to align physician care delivery across the network.
Table 1: Definitions of Contracting Deal Points

Conclusion
Financial incentives drive efforts and thus performance. Intelligent and aligned contracting efforts as well as targeted contract components are essential ingredients to link value to sustainability for all stakeholders involved. When properly deployed, these incentives are a powerful tool in improving the health outcomes of members, increasing patient satisfaction, defining physician role clarity, and managing the total cost of care. Conversely, if not deliberately managed, these same elements can erect challenges that can undermine or even destroy value for those endeavoring to drive value in their organizations and networks.
Look out for the final part of this series, where we dive into the operational alignment needed to reap the value of financial incentives and meet the directives doled out by governance under value based payment arrangements.

