On December 18, 2024, CMS announced that Oklahoma (statewide) and Michigan, New York, and South Carolina (sub-state regions) were accepted to participate in the Innovation in Behavioral Health (IBH) model. IBH is a new state-based model in which states are awarded $7.5 million to invest in specialty behavioral practices that serve the Medicaid and Medicare populations with an acute focus on collaboration with primary care providers. Integrated patient care will include behavioral health, physical health, and health-related social needs (HRSN) to provide whole-person care for patients with moderate to severe mental health and/or substance use disorders (SUDs). Below are 5 key things to know for providers considering participation:
1. Eligibility
Participants must be specialty behavioral health practices, including safety net providers, community mental health centers, opioid treatment programs, and public or private practices who meet the following criteria to participate in the model:
- Licensed by the state to deliver BH services (either mental health and/or SUD);
- Meet any state-specific Medicaid provider enrollment requirements and be eligible for Medicaid reimbursement; and
- Provide mental health and/or SUD services at the outpatient level of care to adult Medicaid beneficiaries (age 18 or older) with moderate to severe BH conditions.
Behavioral health practices serving only Medicare beneficiaries are not eligible to participate in the IBH Model. At a minimum, all Practice Participants must serve Medicaid beneficiaries, however if serving Medicare beneficiaries as well, they may participate in both Medicaid and Medicare components of the model. Federally Qualified Health Centers (FQHCs) and FQHC Look-Alikes that provide specialty behavioral health services are eligible.
2. Responsibilities of Model Participants – Care Delivery Framework
The model’s care delivery framework includes three key levers that are critical for achieving model goals to improve quality outcomes, value-based care, and overall global risk performance.
- Care Integration – Care model must focus on screening, assessing, referring, and treating patients, as needed, for the services they require
- Care Management – Lead an interprofessional care team responsible for identifying and addressing the multi-faceted needs of patients and provide ongoing care management
- Health Equity – Develop a health equity plan (HEP) stipulating how the practice participant will address disparities that impact their service populations
Health information technology, including analytics, reporting, data sharing, and practice transformation, including workflows and staffing, are critical to enabling successful implementation of the care delivery framework.
3. Timeline
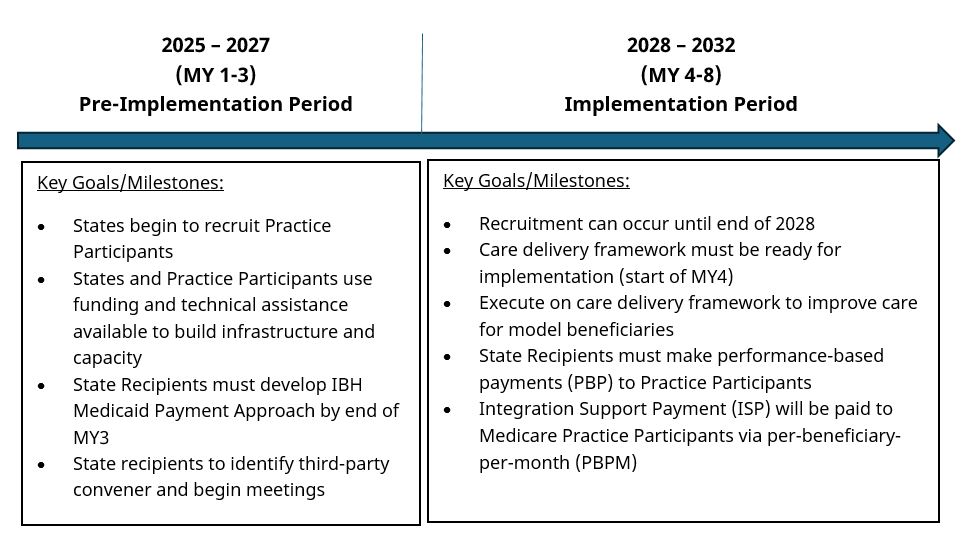
The model will operate for eight years beginning on January 1, 2025.
4. Funding Available
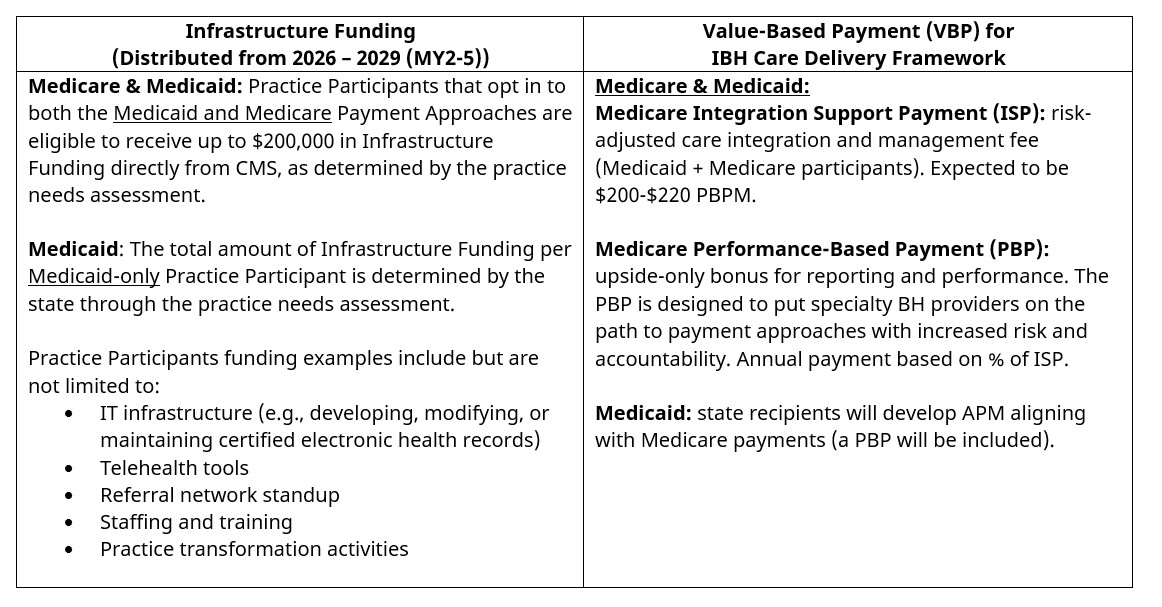
There are two types of funding available for Practice Participants:
5. Implications and Overlaps with Other Models
Practice Participants should evaluate and leverage opportunities to participate in IBH while continuing to participate in existing models.
- Certified Community Behavioral Health Clinic (CCBHC) – participants are allowed to participate in both the CCBHC model and IBH
- Providers participating in IBH are not permitted to participate in Advancing All-Payer Health Equity Approaches and Development (AHEAD), Making Care Primary (MCP) or Transforming Maternal Health (TMaH)
COPE Health Solutions’ team of experts can help your organization position itself for success in the IBH model as well as other value-based care programs through health plans, CMS and state-based 1115 Waiver amendments. Contact info@copehealthsolutions.com to learn how we can help your organization.



