On September 5, 2023, CMS released a new, voluntary state total cost of care model called the States Advancing All-Payer Health Equity Approaches and Development (AHEAD) Model. CMS plans to collaborate with states to increase investment in primary care, improve overall population health, advance health equity, and curb the growth of health care costs. States will apply to CMS to be accepted into AHEAD and engage state health agencies, including state Medicaid agencies, as critical stakeholders. Up to eight states or sub-regions of states will be accepted.
The AHEAD model builds off demonstrations in Vermont, Maryland, and Pennsylvania and encourages a state-level, multi-sector approach to care that both holds states accountable to state or region-specific Medicare and all-payer cost growth targets while increasing investment in primary care. The model is designed to engage all payers in the state over time, including Medicare, Medicaid, commercial insurers, and self-insured employers. For many health systems thinking about opting into the AHEAD model, it is a good time to begin to assess their capabilities, resources (financial and workforce), and needs of the communities they serve.
Additionally, here are 5 key considerations that health systems in potential participating states should be aware of:
1. Model and Application Timeline and Federal Award Amounts
States or sub-regions of states, including Washington, DC, not already selected for Making Care Primary (MCP), are eligible to apply for AHEAD. The AHEAD model is scheduled to operate for a total of 11 years, from 2024 – 2034. States applying to AHEAD will be required to select one of three cohorts depending on readiness to implement the model:
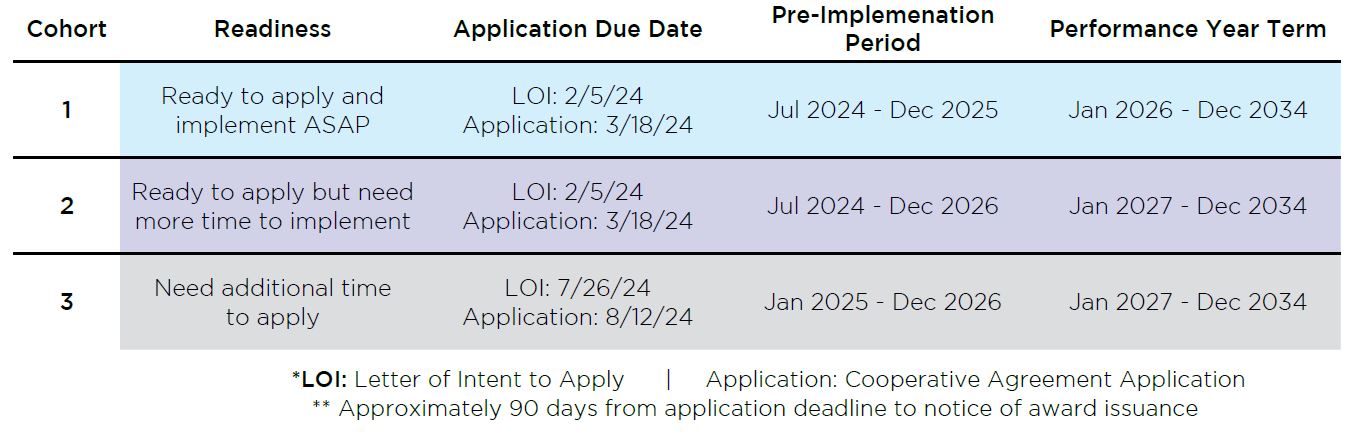
CMS anticipates awarding up to eight states an award of up to $12 million each.
2. Primary Component #1 of AHEAD – Statewide Accountability Targets
- Cost growth targets for Medicare FFS and other line of business costs and quality will be set collaboratively between payers, providers and community.
- Participating states will be required to collect and report statewide quality, health equity, and all-payer TCOC and primary care investment performance data.
- States will be required to select quality and population health measures from a CMS provided set and to set specific targets for each selected measure, with CMS approval, that they will be accountable for meeting.
- Hospitals will remain accountable for performance in CMS’ Hospital-Acquired Condition Reduction Program (HACRP), Readmissions Reduction Program (HRRP), Inpatient Quality Reporting Program (IQR), Hospital Outpatient Quality Reporting Program (OQR), and Hospital Value-Based Purchasing Program (VBP).
3. Primary Component #2 of AHEAD – Hospital Global Budgets
- Hospitals may voluntarily participate in global budgets, however a minimum of 10% of a state or sub-state region’s Medicare FFS hospital net patient revenue (NPR) must be under a hospital global budget by the start of the first performance year, increasing to 30% in the fourth performance year.
- Global budgets will be set prospectively, covering inpatient and outpatient services for a hospital.
4. Primary Component #3 of AHEAD – Primary Care
- Primary care practices, FQHCs, and RHCs that are located within a participant state or sub-state region and are participating in the state’s Medicaid Primary Care Alternative Payment Model (APM).
- Primary Care AHEAD participation will be at the organizational level.
- Hospital-owned practices will only be eligible to participate in Primary Care AHEAD if the affiliated hospital is participating in AHEAD hospital budgets for that performance year.
- Includes enhanced investment dollars and quality measure requirements.
- Must also participate in State’s Medicaid alternative payment model (APM).
5. Health Equity and Behavioral Health Integration
- Each state in the AHEAD program will be required to develop a Statewide Health Equity Plan that will inform statewide equity strategies.
- In addition, participating hospitals will need to create hospital health equity plans.
- Addressing social determinants of health/health-related social needs: The model will also support states in addressing the social determinants of health, such as housing, food security, and transportation, which play a major role in health outcomes.
- States will select at least one behavioral health specific goal.
If you are interested in learning more about AHEAD, please reach out to Allen Miller at amiller@copehealthsolutions.com or Steven Hefter at shefter@copehealthsolutions.com or 213-259-0245 to learn how CHS can help your organization succeed in AHEAD or any other form of value based payment for Medicare, Medicaid or commercial lines of business.
To learn more about how Ankura can help your healthcare organization prepare for and navigate through financial and operational challenges, regulatory changes, and new reimbursement models and reforms, please contact Patrick Pilch at patrick.pilch@ankura.com or 516-301-1470.


