How CMS Is Sequencing Rural Health Transformation for Value-Based Care Success
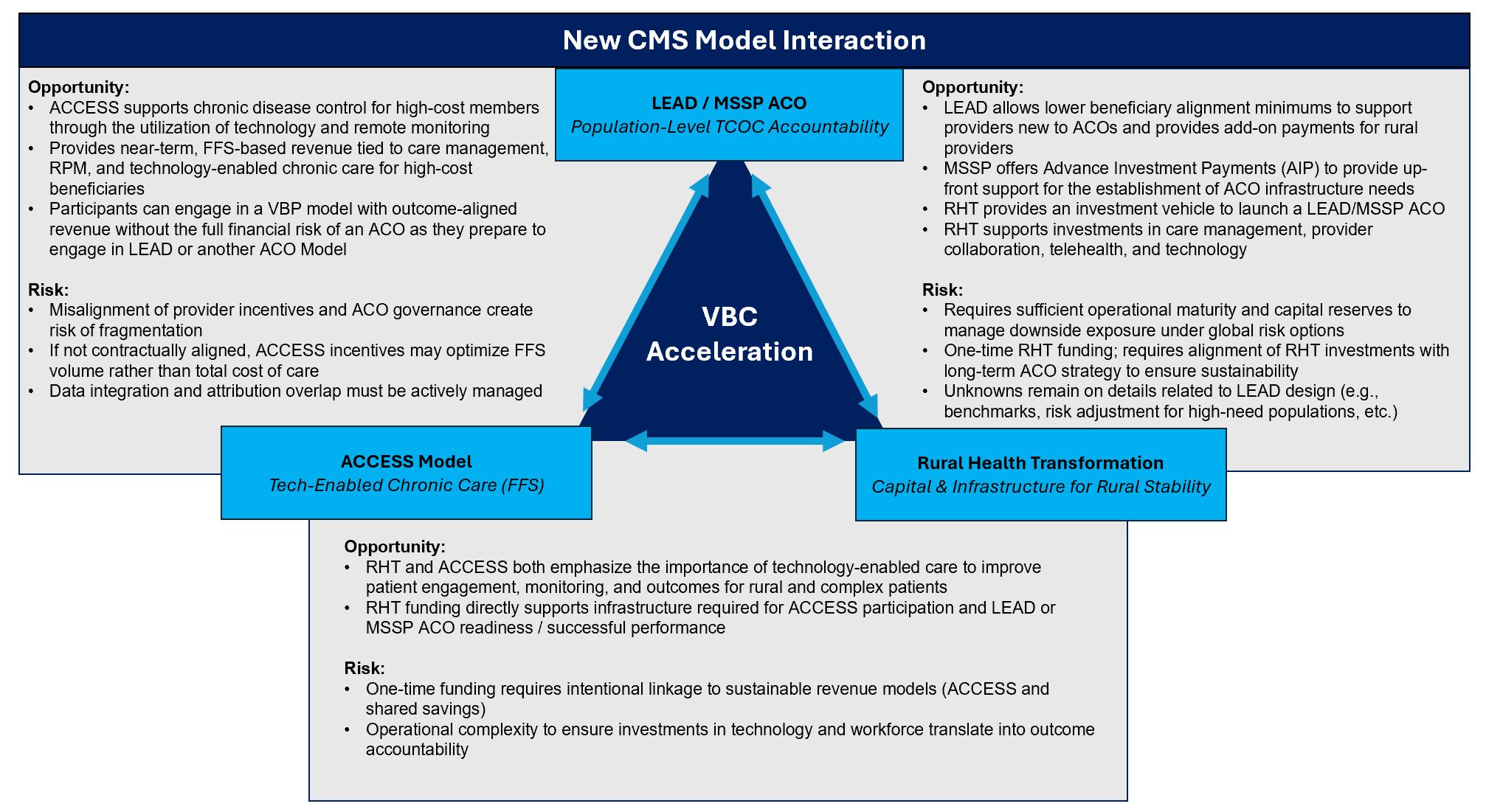
The next phase of rural health transformation is not being driven by a single payment model, but by the intentional interaction of multiple CMS initiatives, each designed to address a different barrier to value-based care.
On December 29, 2025, the Centers for Medicare & Medicaid Services announced that all 50 states would receive funding under the Rural Health Transformation (RHT) Program. This five-year initiative will distribute $50 billion nationally, beginning in 2026, to strengthen and modernize rural health care delivery. New York alone is slated to receive over $212 million in the first year.
At the same time, CMS has introduced complementary models, most notably ACCESS and LEAD, that when viewed together, reveal a cohesive national strategy to move rural and safety-net providers toward sustainable value based payment.
Taken together, Rural Health Transformation (RHT), ACCESS, and LEAD, as well as the existing MSSP ACO advanced investment program (AIP), form a clear and deliberate progression:
Capital & infrastructure → Operational activation → Population-level financial accountability
This sequencing, designed by CMS and operationalized through state strategies like New York’s, creates a powerful VBC acceleration pathway for rural and safety net providers.
- RHT stabilizes the delivery system by providing risk-free capital to strengthen infrastructure, workforce, and technology
- ACCESS activates care delivery by enabling FFS-based, technology-supported care management through partnerships with technical and care management organizations
- LEAD / MSSP ACO introduces population-level accountability, converting operational performance into shared savings or losses
Together, these programs form a structured on-ramp to sustainable value based payment in rural markets.
RHT plays the foundational role. New York’s application makes clear that this program is not intended to drive utilization or short-term performance improvement. Instead, RHT provides no cost capital to stabilize vulnerable providers and address long standing gaps in care coordination, workforce capacity, technology infrastructure, cybersecurity, and regional collaboration. These are precisely the elements that fee-for-service reimbursement has historically failed to support, yet they are prerequisites for success under any population based model.
For providers, this distinction matters. RHT funding should not be viewed as a traditional grant, but as pre-paid value-based care infrastructure. Its purpose is to reduce operational fragility and enable population centric delivery models that can later support accountability. An effective RHT investment should measurably reduce future PMPM volatility, improve attribution stability, and decrease fragmentation across the care continuum. If it does not, it is unlikely to be sustainable once the funding period ends.
What does this mean for providers in New York?
In New York, the opportunity created by this grant is amplified by the concurrent launch of the state’s Safety Net Transformation Program. Beginning in State Fiscal Year 2025, the Safety Net Transformation program opened funding to support safety-net hospitals in improving access, equity, quality, and financial sustainability through collaborative partnerships. For safety-net facilities serving rural populations, the combination of Safety Net Transformation funding and RHT capital creates a rare opportunity to stabilize finances while simultaneously building the infrastructure required for long-term participation in value-based care.
When layered together, RHT and Safety Net Transformation funding can support workforce investments, technology modernization, and regional integration. Coordinated efforts with ACCESS providers can then be used to operationalize care management and patient engagement. Over time, this combination positions rural Safety Net providers and partnering ACCESS organizations to participate confidently in LEAD or MSSP ACO and to generate performance-based returns that extend beyond the grant period.
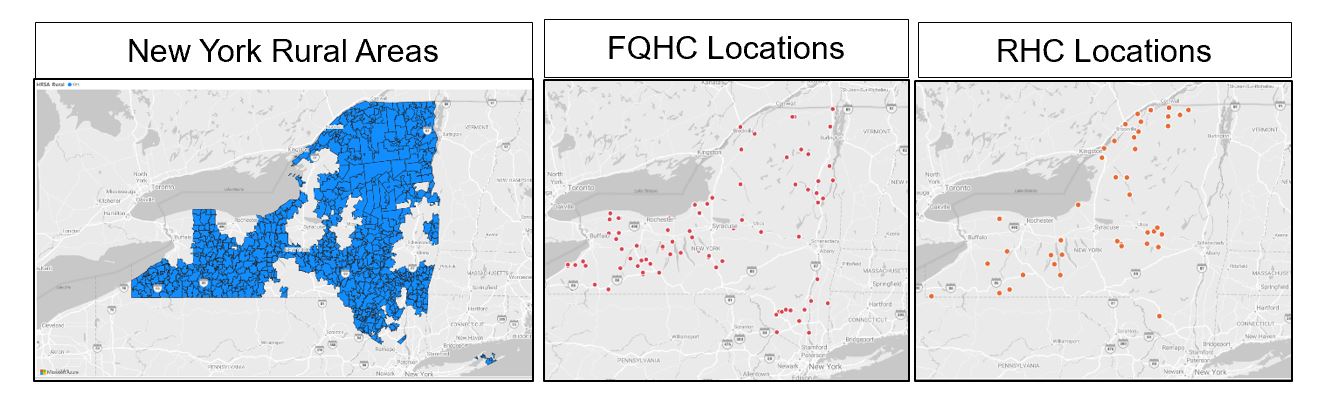
This framework is also well suited to Federally Qualified Health Centers, which already function as population anchors in many rural communities. Their stable payment structures allow them to tolerate transformation work while expanding care management and virtual care capabilities. Rural Health Clinics, while often more constrained by scale and capital, can similarly leverage this progression by participating in regional partnerships that distribute accountability across multiple providers. Visuals below show how critical FQHCs and RHCs are in key rural areas. Integrated rural networks will require engagement and co-development with these clinics for success:
Community-based organizations and Social Care Networks established under New York’s 1115 waiver also have an important role to play. By addressing social drivers of health and supporting patient engagement, these networks can complement clinical care management and enhance the effectiveness of ACCESS-enabled interventions. RHT and related funding streams offer these organizations the capital needed to expand infrastructure and integrate more deeply into population health strategies.
Ultimately, New York’s Rural Health Transformation Plan is about alignment. Providers that understand how RHT, ACCESS, and LEAD/MSSP ACO reinforce one another can turn geography into strategy, infrastructure into leverage, and population focus into sustainable value-based success. Those that pursue these programs in isolation risk achieving short-term gains without long-term impact.
How to Prepare
Now is the opportunity for providers to take deliberate steps that will position themselves for successful participation in this program. Organizations and providers alike should begin to:
- Assess their readiness, including data infrastructure, quality reporting capabilities, and population health management capacity.
- Strengthen regional partnerships across hospitals, FQHCs, clinics, behavioural health providers, SCNs and community partners to support coordinated, ecosystem level strategies.
- Align with Medicaid financing and other grant funding (i.e. Safety Net Transformation Program) to ensure RHT initiatives complement existing funding
- Plan for accountability and sustainability, with a focus on measurable outcomes, operational efficiency, and reinvestment beyond the funding period.
COPE Health Solutions supports stakeholders across all four areas through a combination of strategic consulting services and its ARC Population Health Management Platform. Our expertise helps rural providers evaluate readiness, align regional strategies, operationalize performance measurement, and build sustainable care models that are positioned for success within this state specific and other federal initiatives.
For more information and to talk through your organization’s next move, reach out to us at info@copehealthsolutions.com or visit us at copehealthsolutions.com.