Federal Framework Impacting Texas Transformation
Texas is entering a new era of rural health that will be shaped by the federal Rural Health Transformation (RHT) Program, led by the Centers for Medicare & Medicaid Services (CMS). This program represents the largest coordinated federal investment in the nation’s rural healthcare system to date and is an accountability driven effort that is focused on reshaping how rural care is delivered, financed, and sustained over time. On December 29, 2025, CMS announced that all 50 states would receive funding awards through the RHT Program. This five-year initiative will distribute $50 billion nationally to strengthen, modernize, and stabilize rural health systems across the country. Beginning in 2026, states will receive their first year of funding, with Texas slated to receive the largest distribution of $281 million.
Through Rural Texas Strong: Supporting Health and Wellness, Texas clearly articulated both the need for focused investment and a comprehensive strategy designed to reach 100% of the 202 rural counties in the state. This project narrative documents the challenges rural Texas healthcare providers and patients face daily:
- More than 500,000 rural Texans must travel an hour or more each way to access higher-level care, with some areas in West Texas exceeding 100 miles to reach specialty services.
- Rural Texans experience higher rates of heart disease, cancer, stroke, and unintentional injury when compared to Texans in urban areas.
- These disparities create significant economic impact, with preventable health conditions costing the state economy nearly $7 billion annually.
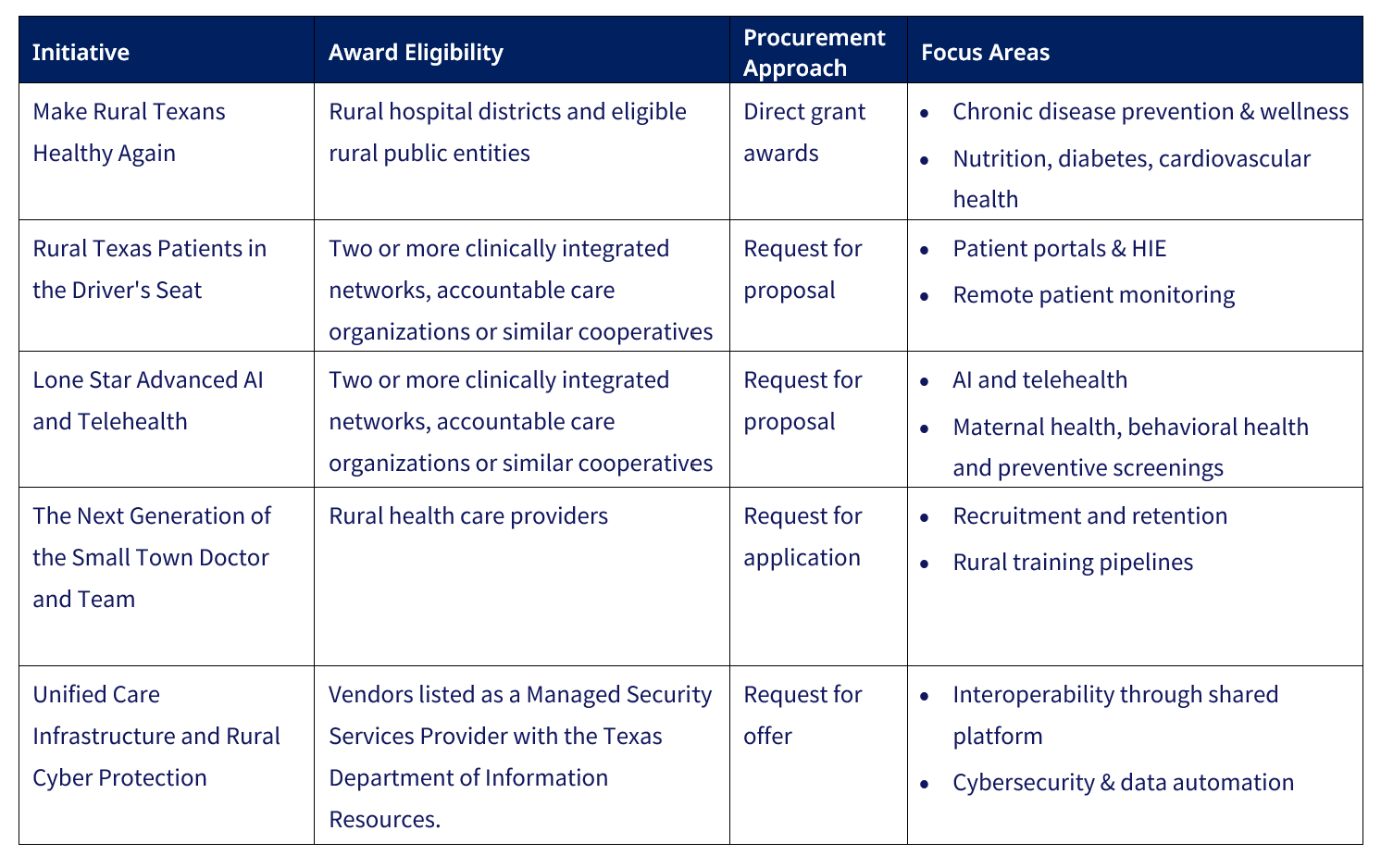
The strategy developed by Texas is a system-level transformation effort and not intended for short-term relief. The state’s RHT plan builds upon federal priorities while introducing six uniquely Texas strategies designed to work together across access, workforce, technology, and financial stability:
Stakeholder Implications
While this funding offers significant opportunity for rural healthcare providers, it also requires that they operate differently than previous grant funding opportunities. Providers need to understand and be able to articulate how their unique role fits into a larger regional strategy that supports the program’s system-level emphasis on integration, data, and measurable outcomes.
As they do now, rural hospitals will serve as anchors for access, workforce stabilization, and care coordination. Funding priorities around financial solvency, service line preservation (including obstetrics and behavioral health), technology modernization, and cybersecurity will favor hospitals that can demonstrate regional collaboration and measurable improvement. Additionally, RHT dollars are intended to complement, not replace, Medicaid and Medicare financing, requiring hospitals to clearly align funding strategies.
FQHCs, FQHC look-alikes and rural health providers will remain critical access points for prevention, chronic disease management, and integrated primary and behavioral health care. Through these initiatives providers should expect increased importance on data sharing, patient engagement technology, workforce pipelines, and partnerships with rural hospitals and clinics. Participation will increasingly require standardized reporting and alignment with regional strategies rather than stand-alone operations.
How to Prepare
Now is the opportune for providers to take deliberate steps that will position themselves for successful participation in this program. Organizations and providers alike should begin to:
- Assess their readiness, including data infrastructure, quality reporting capabilities, and population health management capacity.
- Strengthen regional partnerships across hospitals, FQHCs, clinics, behavioral health providers, and community partners to support coordinated, ecosystem-level strategies.
- Align with Medicaid financing and Directed Payment Programs (DPP) to ensure RHT initiatives complement existing reimbursement and quality frameworks.
- Plan for accountability and sustainability, with a focus on measurable outcomes, operational efficiency, and reinvestment beyond the funding period.
COPE Health Solutions supports stakeholders across all four areas through a combination of strategic consulting services and its ARC Population Health Management Platform. Our expertise helps rural providers evaluate readiness, align regional strategies, operationalize performance measurement, and build sustainable care models that are positioned for success within this state specific and other federal initiatives.
Additional Federal Signals: ACCESS Model, and LEAD ACO Program
In addition to rural health transformation, Texas providers should be aware of the newly announced ACCESS Model and the LEAD ACO Program, also CMS initiatives that reinforce the similar principles of accountability, technology-enabled care, equity, and value-based payment. While distinct from RHT and Texas’ DPPs, these models further signal the direction of future federal policy. More information regarding the ACCESS Model and Lead Programs can be found in our federal healthcare policy update .
Bottom Line
For Texas rural providers, hospitals, and FQHCs, the question is no longer whether funding and no cost investment exists, but instead whether organizations are positioned to meet the accountability, equity, and performance expectations included in RHT and further reinforced by broader federal reforms. Early preparation, strong regional partnerships, and alignment with Medicaid financing strategies will determine which rural systems translate this historic investment into lasting impact.
For more information and to talk through your organization’s next move, reach out to us at info@copehealthsolutions.com or visit us at copehealthsolutions.com.

