1. Evaluate your practice’s capacity to meet the three domains of MCP’s care delivery approach*: care management, care integration, and community connection
- Care management: focus on designing and developing care management and chronic condition self-management services, with an emphasis on chronic disease prevention and management
- Care integration: strengthen connections with specialty care (Track 2 and 3 participants are required to form “collaborative care arrangements” with specialty care partners) and focus on managing behavioral health conditions, including staffing and workflows for a behavioral health integration approach
- Starting in Track 2, practice participants will access a new MCP-specific e-Consult code
- Community connection: implement screening tools, workflows, and partnerships with social service providers (i.e. CBOs) to address health-related social needs (HRSN)
- Leverage community health workers (CHWs) or equivalent staff to operationalize workflows
* Practices must meet the care delivery requirements in their starting Track by the end of PY2 (12/31/25)
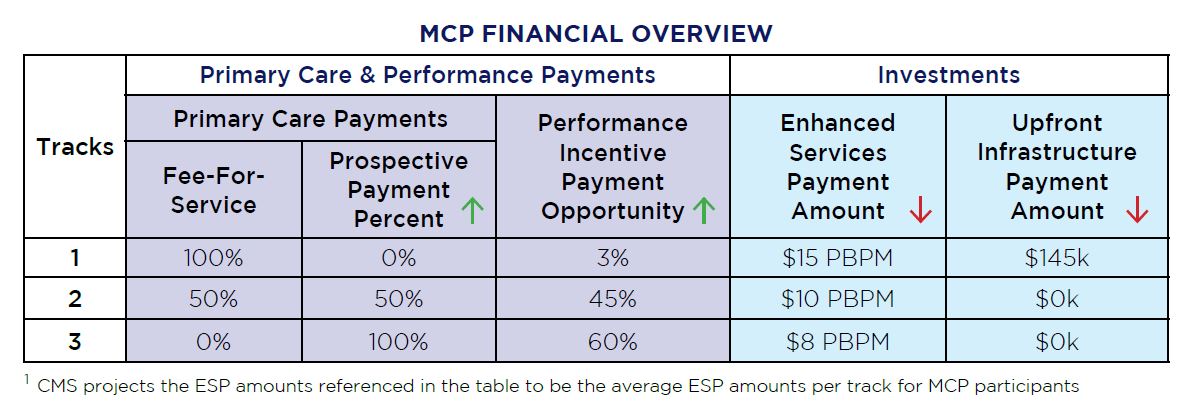
2. Evaluate financial implications to your practice by modeling the six new MCP payment types; your practice’s track will determine eligible payments
- Upfront Infrastructure Payment (UIP) for Track 1 only – lump sum payment of $72,500 in 2024 and $72,500 in 2025 – determine if your practice is eligible
- CMS has indicated that there are three allowable uses of these funds: 1) increased staffing, 2) SDOH strategies, and 3) health care infrastructure, including health IT infrastructure
- Eligible Track 1 participants must develop a UIP Spend Plan to be submitted to CMS during summer 2024
- Enhanced Services Payment (ESP) – quarterly, prospective PBPM payment adjusted for attributed population’s* risk level for care management activities
- Prospective Primary Care Payment (PPCP) – quarterly payment based on historical primary care spending – Track 1 continues to bill FFS and payments move toward prospective payments from Tracks 2 to 3
- Performance Incentive Payment (PIP) – based on performance on the MCP Performance Measure Set (a set of quality and cost measures), practices may earn an upside-only adjustment on FFS and PPCP payments across all tracks
- MCP e-Consult code – available to practice participants in Tracks 2 and 3
- Ambulatory Co-Management – only available to specialty care partners for practice participants in Track 3
* CMS provide each practice with its list of attributed Medicare beneficiaries and will update every quarter
3. Begin to develop your practice’s Health Equity Plan – submission due in October 2024
- Practices will use a template provided by CMS, and practices will report on progress throughout the model period
4. Evaluate data and IT resources provided by CMS and remaining gaps to achieve MCP model goals
- Expanded data feedback reporting (eDFR) is a tool to provide participants with insights into their attributed beneficiary population, and CMS will also provide performance data on specialists
- States will also provide data aggregation and HIE resources
- Data collection is critical, as practice participants will be required to collect and report on demographic and HRSN data for quality measure and care delivery reporting – health IT requirements center on data and interoperability, and MCP participants are required to connect to a regional or national HIE
- Sociodemographic reporting due to CMS in July 2025
- Quality reporting due to CMS in January 2026
5. Evaluate Track movement options and overlap options with other CMMI models
- Participants who enter Track 1 may remain for 2.5 years before moving to Track 2
- Participants who enter Track 2 may remain for 2.5 years before moving to Track 3
- Participants who enter Track 3 may remain for entire remainder of model period (until 2034)
- Overlap with MSSP allowed only from July-December 2024 – but providers needed to have withdrawn from SSP before the June 2024 SSP provider roster submission deadline (if in both models in 2024, no MCP payments will be made)
- Other than this, MCP practices generally will not be able to participate in other CMMI models, and MCP practices will need to monitor the providers listed on their participating provider lists to properly manage the correct model in which each physician and their attributed lives reside
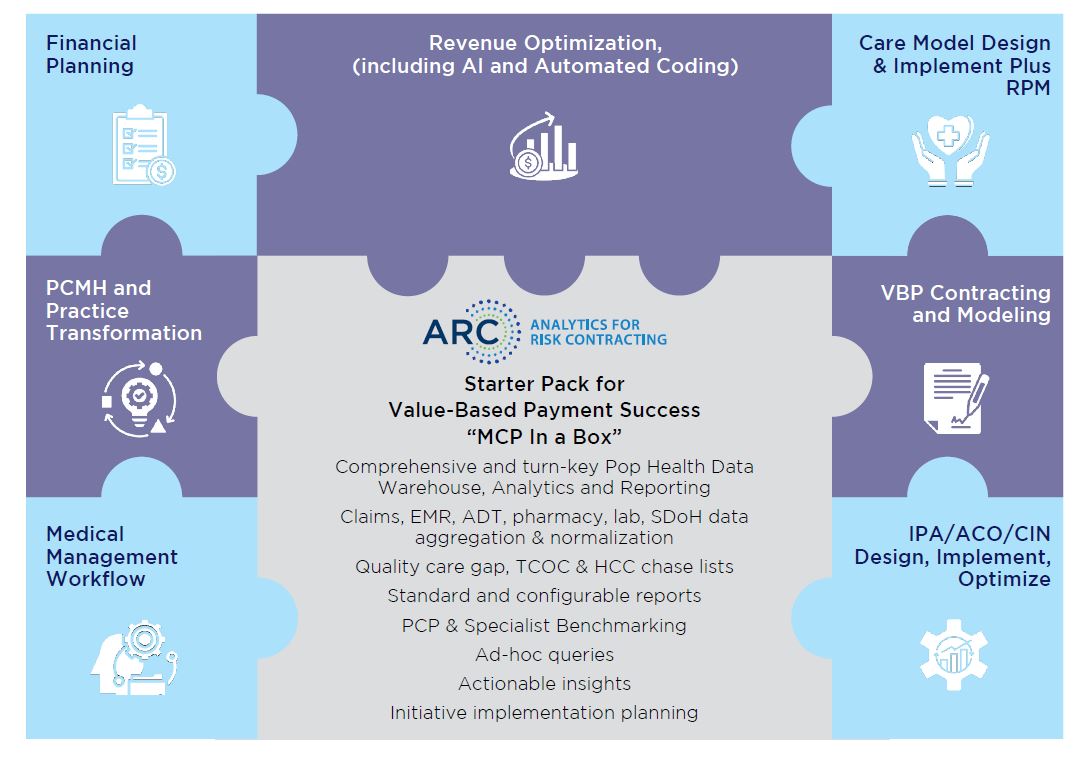
How we can help: leverage the graphic below that we used in our previous thought leadership articles