On June 8, 2023, CMS announced a new CMMI primary care model, Making Care Primary (MCP), covering traditional Medicare beneficiaries, that aims to strengthen primary care infrastructure through service delivery and care integration enhancements designed to improve an MCP entity’s care management programming, specialty care integration and community supports connections closing social determinant of health gaps. The program is meant to provide a progressive roadmap into value-based payment (VBP) arrangements for primary care clinics with limited VBP experience.
CMS will publish a MCP Request for Application (RFA) in August with a November MCP application submission deadline.
5 key considerations for health care stakeholders interested in MCP:
1. VBP Experience Flexibility & Growth Path
- CMS encourages and supports model participation for primary care clinics with limited value-based payment experience, including FQHCs and safety-net providers, through three progressive tracks (see MCP Participation Track Overview Table below).
- CMS has frequently cited FQHCs, safety-net providers and independent primary care clinics as primary examples of provider types for whom the MCP was designed.
- MCP provides novel opportunities for entities beyond its three progressive tracks: this is the first opportunity provided to FQHCs to participate in a multi-state advanced primary care model.
- All MCP entities must meet CMS eligibility criteria to participate in the model.
- Entities eligible to participate in MCP are legally formed, Medicare-enrolled entities billing health services to a minimum of 125 Medicare beneficiaries with a majority of its physical office settings in an MCP test state (CO, MA, MN, NC, NJ, NM, NY, WA).
- Entities not eligible to participate in MCP are rural health clinics, concierge practices, current Primary Care First (PCF) practices, current ACO REACH participant providers, grandfathered tribal FQHCs. Entities also may not concurrently participate in MSSP after the first six months of MCP Primary Care advancement.
- CMS has frequently cited FQHCs, safety-net providers and independent primary care clinics as primary examples of provider types for whom the MCP was designed.
- CMS will require MCP participants to progress through the three tracks of the program until they reach Track 3
- MCP Participants in Tracks 1 and 2 must progress to the subsequent track in a timeframe yet to be determined.
- There are presently no time limits for MCP Participants in Track 3.
2. Primary Care Advancement
- CMS will provide MCP entities in all three tracks with prospective, risk-adjusted enhanced services payments to support primary care advancement.
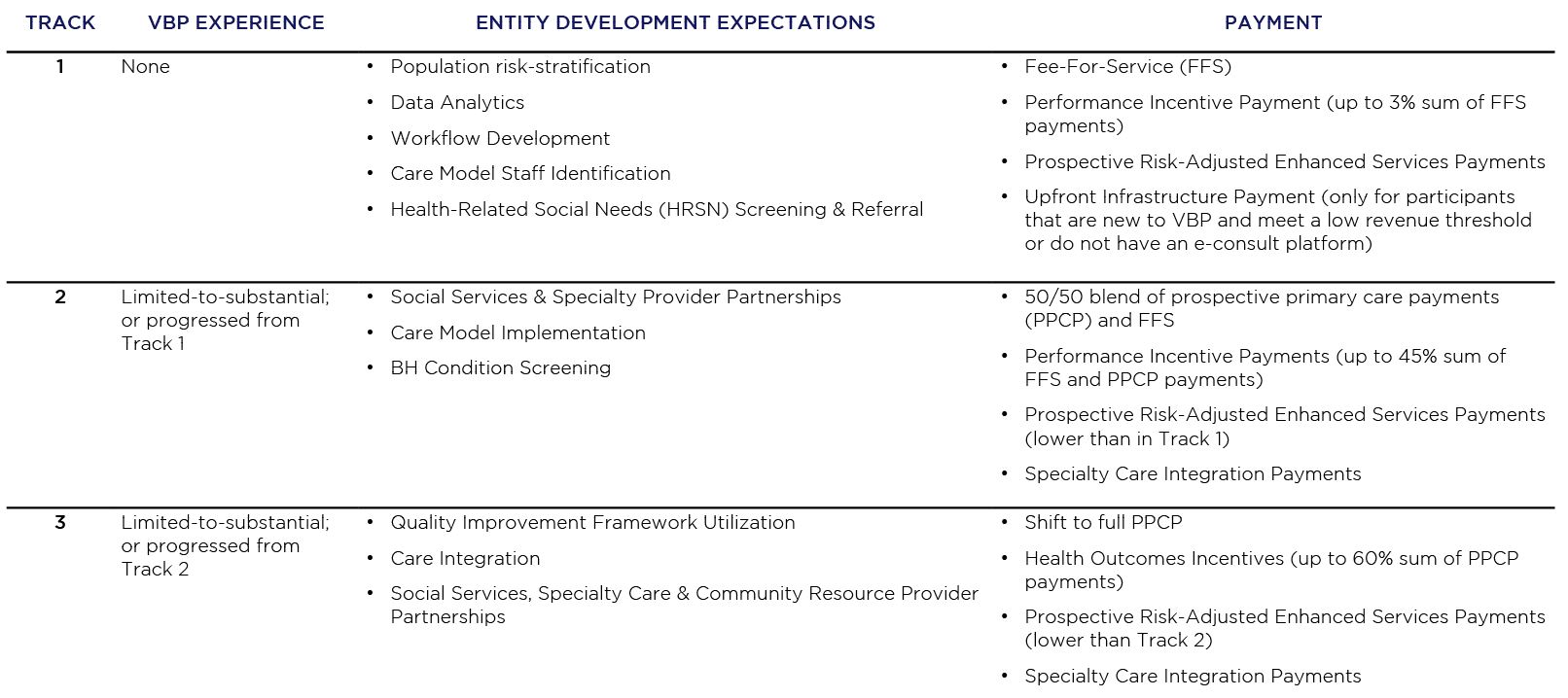
- The MCP Participation Track Overview Table (shown in Figure 1) provides an overview of the parameters governing the three progressive tracks in which MCP entities may participate in the model:
- Previous level of VBP experience
- MCP entity development expectations
- Payment arrangement
- Enhanced services payments will support the development of three core primary care service delivery capabilities:
- Care management development with a focus on chronic condition self-management
- Specialty care integration while leveraging behavioral health screenings
- Community supports and services partnerships to address a patient’s health-related social needs (HRSNs)
- The MCP Participation Track Overview Table (shown in Figure 1) provides an overview of the parameters governing the three progressive tracks in which MCP entities may participate in the model:
3. Health Equity
- CMS will continue their efforts to achieve health equity through requirements and provisions throughout the model.
- MCP participants will be required to do the following:
- Develop a “Health Equity Plan”, akin to those required in ACO REACH
- Implement HRSN screening and referrals
- CMS will do the following:
- Permit MCPs to reduce cost-sharing for patients in need
- Adjust payments by clinical indicators and social risk
- Measure the percentage of patients screened for HRSNs
- Collect data on certain demographic information and HRSNs to evaluate health disparities in MCP communities
- MCP participants will be required to do the following:
4. Payer Program Alignment
- CMS has committed to working with State Medicaid agencies to align MCP with state programs and engaging with private payers to extend MCP alignment across lines of business (LOBs).
- MCP alignment efforts will extend to the following:
- Streamlining core quality measure across payers and CMMI programs and the testing of new and innovative measures.
- Sharing state and national level resources with MCP participants, including practice and patient-level data
- Providing support for success across MCP activities, including, but not limited to, state-level data aggregation and reporting, specialty care data, practice coaching and peer-to-peer learning
- MCP alignment efforts will extend to the following:
5. Decade-Long Term
- CMS announced a 10.5 year-long term for the program, from July 1, 2024, through December 31, 2034, amongst the longest initial proposed term in a CMMI model in recent years.
- CMS will begin accepting applications for MCP later this summer.
Making Care Primary (MCP) Participation Track Overview Table (Figure 1)
Your Trusted Partner for VBP Success
COPE Health Solutions (CHS) is a national tech enabled services firm with unparalleled CMS, CMMI and State Medicaid Waiver model experience that leverages deep expertise, proven tools, and processes across key VBP functions to drive success for all delivery system stakeholders.
CHS is prepared to support the development of your organization’s key VBP domains listed below for success in the MCP and its alignment with its programs across all LOBs, including Medicare FFS, MA, Medicaid, Employer-Sponsored Plans and Commercial insurance.
Key VBP Domains
Value-Based Payment Assessment and Roadmap
- Alignment around vision and priority 3-5 year goals for Medicare FFS and other lines of business including Medicare Advantage, Dual Eligible (D-SNP, C-SNP, PACE), Medicaid Managed Care, Commercial and Direct to Employer as applicable
- Assessment of fit and requirements for success in the MCP model, including establishment of the right legal, governance and contractual frameworks to succeed in financial risk not only for MCP but also in VBP contracts with health plans
- Detailed implementation plan with key milestones and expected ROI
Value-Based Payment Network and Contracting
- VBP success through optimal network design and management, funds flow, care management and quality improvement, data management and provider engagement strategies, as well as contracting with payers other than CMMI/CMS to align various payers around your VBP roadmap
Data Aggregation and Analytics
- Proven population health management data warehouse and analytics platform with EMR integration capabilities and easy to use benchmarking and PCP dashboarding tools with provider and member specific chase lists
- Risk stratification and performance measure reporting critical to delivering actionable data
- Integration of SDOH data for risk stratification and leveraging of community based organizations
Specialty Care Network Contracting and Workflow Optimization
- Analytics and benchmarking to identify the highest performing specialists for targeted referrals
- Proven e-consult workflows and evidence based best practice care guidelines
Provider Engagement
- Provider engagement and education on MCP, care management and performance review for opportunities integral to success under MCP and the participant’s other VBP contracts
- Practice transformation and improved performance on quality and total cost of care goals
- Physician portal and best practice actionable data
Care Management
- Evidence based best practices for care management programming development, staffing models and implementation including beneficiary health-related social needs (HRSN) evaluation & risk stratification into appropriate levels of care that are critical to improving quality & equity outcomes
Member Engagement
- Proven member engagement app integrated with analytics to support specialty self-referral, chronic disease self-management and access / navigation
Workforce Development
- Rapid implementation, scalable recruitment, training and education and retention programs for medical assistants, care coordinators, nurse practitioners, physician assistants and other essential roles
Contact us at info@copehealthsolutions.com to learn how we can help your organization apply and get approved into the new program.


