 A push towards pay-for-performance
A push towards pay-for-performance
The term “pay-for-performance” (P4P) has matured in healthcare over the last decade from concept to reality as healthcare policy creators, administrators, and clinical providers work together to develop a more efficient, sustainable, and quality healthcare system focused on the patient. While Medicare demonstration projects and Medicaid Waivers have been around for many years, more recently there is a large focus on pay for performance incentive programs in healthcare transformation. These require providers to be able to demonstrate successful achievement of defined process and clinical measures in order to earn shared savings and/or incentive payments; both efforts made to change the way care is delivered across the care continuum and result in actual quality and cost outcomes.
The most notable push towards P4P is seen in a number of implementation requirements and quality goals of the Affordable Care Act (ACA), which was passed in 2010. Acknowledging the unsustainable cost of healthcare in the US, the ACA allows for a number of demonstration and pilot projects focused on P4P as a conceptual model to assist in the challenging operationalization of policy goals and concepts related to provider reimbursement practices, quality of services provided, health of the overall population, and reductions in overall spending. ACA demonstrations and pilot examples include the National Pilot Program on Payment Bundling, Wellness Program Demonstration Project, Community Based Care Transitions Program for high risk Medicare Patients, and many more. These incentive dollars are generally considered investment, or transitionary, funds that allow providers the ability to make incremental changes in operational and clinical practices to support the transition from fee-for-services payments to value-based and capitated payments This shift in payment structure rewards providers for meeting, all or in part, specified process and clinical outcomes rather than paying for services rendered. The intent is to enhance the overall patient experience beginning with the physician encounter to improvements in individual health status.
Pay-for-Performance in Medicaid
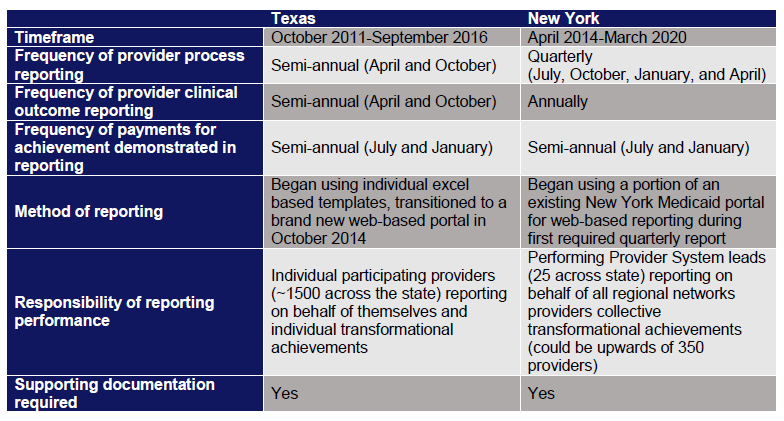
Over the past decade CMS has worked with states to develop P4P demonstrations for the Medicaid population. One vehicle for this work has been the Delivery System Reform Incentive Payment (DSRIP) programs seen in some states’ Section 1115 Medicaid Waivers. Individual states are charged with not only developing program requirements for performance but also designing and implementing a robust reporting and monitoring system for participating providers in order to draw down incentive funds. The two largest and most complex active DSRIP programs with relation to structure and inclusion of provider types across the care continuum are found in Texas and New York. Each state has extensive clinical and process improvement performance expectations for their providers. Both of these states have comparable expectations of providers despite different approaches to their
actual timing and processes of reporting (more information below), however New York’s program is groundbreaking in its statewide requirements to achieve execution of 80% value based payment agreements between providers and Managed Care Organizations and regional level reporting of clinical outcomes.
Why is reporting so important?
The current DSRIP programs in Texas and New York are worth up to $11.1 billion all funds and $6.8 billion all funds for five years, respectively. Through these programs, no funds will flow to the providers until they perform the required work to achieve all program requirements and can also successfully document and report this achievement to the state and CMS. Reporting, and reporting well, is a critical factor for success in pay-for-performance programs et al, not just DSRIP. P4P is not limited to DSRIP programs only, as it is now a requirement for Medicaid Managed Care, Medicare, and Commercial plans. Health plans are required by states to report on dozens of quality outcomes each year for their members. In fact, in 2013, health plans in 34 states were required to report on HEIDS (Healthcare Effectiveness Data Information Set) and CAHPS (Consumer Assessment of Healthcare Providers and Systems) measures for all commercial and Medicaid plans for members in the state (NCQA.org). States require the reporting of these measures in anticipation that what is measured will be improved upon over time, to provide consumers with better access to data about the quality of care they can receive, and in order to collect standard data for public health officials to analyze regional differences in healthcare quality.
The quality outcomes required for reporting in DSRIP programs very much align with the quality reporting required by states. For example, 25 of the clinical reporting and performance outcomes in the NY DSRIP Program are also required measures for Medicaid Plans in the 2015 Quality Assurance Reporting Requirements. Just as health plans report on behalf of all members in their service area, the providers under NY DSRIP will report on, and be measured against improvement, for Medicaid members within a region of the state. DSRIP programs allow providers and systems the time and incentive to learn how to be successful for clinical outcome reporting, which will be critical to long-term success and sustainability within the healthcare industry. Systems and geographic regions who leverage DSRIP to develop technology platformas and competencies to collect the right data, and use real-time data to make clinical decisions, while reporting outcomes through health plans along the way will be able to increase total revenue available through improved quality scores and shared savings from reductions in total cost.
Since its inception in 2008, the Triple Aim has moved to the forefront of healthcare professionals’ minds and integrated into operational strategy. Providers need to be able to demonstrate that they can reduce total cost across a system while improving quality and patient satisfaction in parallel. This is a key lesson for anyone participating in a DSRIP or other P4P program – now is the time to put boots on the ground and focus on improvements and reporting. This will enable organizations to be more successful across all lines of business and allow the safety net providers to compete, creating opportunities for financial sustainability in the long term.
The following table provides high-level information to show the similarities and differences in the development and execution of reporting practices in Texas and New York DSRIP programs.
Key drivers to successful reporting in a pay-for-performance environment
-
- Clearly defined processes, communication and accountability
Adapting to P4P requirements can be challenging, for organizations of all size and maturity levels. Without clearly defined processes and accountability not only for reporting, but also performing against required milestones or outcomes, can lead to a number of problems.In working with our clients we have observed a lack of structure for reporting generally leads to delays in collection of reporting requirements, creating a downstream impact on being able to validate if reported results accurately represent performance, and ultimately increase the risk of scrutiny from internal governance and oversight or auditing bodies of the program.The Community Care Collaborative (CCC) in Austin, Texas (a joint venture between Seton Health System and Central Health to deliver integrated care to the safety net population in Travis County) has been very proactive to ensure their success in reporting process metrics under the Texas DSRIP program. Some factors, but by no means all, that have contributed to their success include:- • Putting one person in charge and making them accountable for reporting (reporting manager or champion). This person should be considered a subject matter expert (SME) who understands the complexity of state and federal reporting requirements and can have foresight into ensuring the design of the internal reporting process is in alignment. Additionally, this person must understand how performance and reporting requirements link to incentive funds being received; based on the internal reporting process the SME should be able to anticipate what funds an organization is eligible to earn during a performance period based on performance and quality of reporting.
- • Maintaining frequent, clear communication with providers and the state. This is critical to prevent confusion regarding what should be reported, or how reports should be created. Often reporting requirements change over time and these must be communicated clearly and concisely in order to adapt reporting processes to stay compliant.
- • Working closely with providers to develop clear expectations for reporting. The more clarity regarding expectations of reporting (requirements, timing of report creation, performance windows, expected level of quality for reports, etc.) that is created up front and throughout the program will result in less rework, high-quality reports, and long-term success.
- • Implementing monthly and weekly reporting cycles to refine the practice of reporting. On the onset it may seem as if frequent meetings will take away from the actual work that needs to be performed, but creating on-going accountability to monitor progress is key to adapting program implementation efforts in real time based on what the data or status updates reflect. In these meetings, risks can be raised in a safe environment and barriers can be removed to ensure goals are achieved.
These practices will set an organization up for success for process and clinical outcomes, but are not representative of the full strategy or reporting reality. As the DSRIP program in New York begins to take flight, Preforming Provider Systems (PPS) (a collection of providers within a specific geographic area working together to create an Integrated Delivery System) are looking to use data to implement change within, and across, organizations as they begin to form an Integrated Delivery Systems (IDS). Reporting expectations for clinical outcomes require PPS to collect data on attributed lives, improve their health outcomes, and report the improvement to the state each year.
Finger Lakes Preforming Provider System (FLPPS), a PPS consisting of hundreds of providers across 13 counties in upstate New York, is working diligently to stand up the infrastructure, processes, and accountability to perform well in DSRIP reporting domains. They are going to leverage the reporting capabilities of larger systems within the region, Rochester Regional Health and University of Rochester Medicine, in conjunction with smaller health systems and community IPAs, to build a reporting infrastructure that will enable the PPS to collect clinical data from providers across the care continuum, analyze data against state defined measure specifications, and implement specific improvement initiatives within providers to drive change and produce clinical outcome transformation. If the PPS is able to achieve a 10% improvement in the difference between their collective baseline and a state defined goal, they will successfully draw down payment for their performance. This is not an easy task, but with the right vision, technology pipelines, and focused efforts it is an endeavor well worth pursing; success under Medicaid DSRIP reporting builds a solid foundation in which the providers, individually and collectively, can build upon to improve their reporting practices for Medicare and commercial requirements, enabling the opportunity for long-term sustainability.
- Preparation and validation
The old saying goes, “Measure twice, cut once,” and the same theory applies in preparing reports in pay-for-performance programs. Organizations that take the time to prepare and validate not only set themselves up for a higher success rate in having reporting documentation approved for payment, but also find preparing for and passing future audits much easier than organizations with no formal preparation or validation process for reporting. Some suggestions for organizations to consider to set themselves up for success in this area are:- • Develop a reporting manual that outlines roles and responsibilities of employees, data sources for milestones and metrics, outlines the internal timeline and process as well as portrays any and all guidance produced by the program administration, i.e. CMS.
- • Appoint a reporting manager, or SME, to oversee the reporting and validation process.
- • Appoint a quality assurance officer to compare completed reports to internal and external reporting requirements and sign off when reports meet expectations. This person should not be afraid to not approve a report the first time it is submitted; they should have high expectations of others work.
- • Approach each reporting period as a Plan Do Study Act (PDSA) cycle and continually adapt and improve your reporting process and requirements based on lessons learned and newly released guidance.
- Maintaining flexibility and anticipating the challenges
To continue the examination of success factors, flexibility is the key to preparedness. Organizations should be prepared for reporting and performance expectations to adapt and change overtime as oversight agencies like CMS or departments of health understand more about what they are looking for, witness best practices throughout the program and then place that requirement on all participants.Anticipating challenges, such as delay in receiving guidance or submission templates from oversight agencies is critical. Successful organizations prepare and implement internal reporting processes early on and are prepared to respond in an agile fashion when guidance is received late. The more you can anticipate and plan for, the more successful reporting will be.
- Use data to drive decision making
While reporting processes and expectations may appear to be arduous, proactive organizations look for the value in creating a reporting culture, where data is used to drive decision making. Whether the data is quantitative or qualitative, process or clinical, information is powerful when transforming an organization or system. Some organizations may choose to use daily huddles to analyze information, a tactic seen in Agile approaches to project management. Others may develop homegrown dashboards to review internally and report information, and some organizations are turning to online platforms. The method of data collection, storage, and analysis will differ based on an organizations need, size, capabilities, and reporting requirements of a specific pay-for-performance program.Janet King, Director of the PMO at FLPPS is excited about the data and information that will be available from partners within their PPS. According to her, “The role of reporting is multi-faceted, not only does reporting from partners across the PPS [aggregated by the lead] allow documentation to be sent to New York state to draw down incentive funds, but the information is also going to be a measurement barometer for how well the network is developing and doing.”FLPPS is one of many PPSs in New York who are looking to an online solution to help collect, analyze, and store information specific to the reporting and performance requirements of DSRIP.“While the online tool may be helpful, it won’t be a full solution at first,” notes Janet, “getting everyone to use the tool is going to be a challenge, and our staff is going to have to be flexible with each provider’s vast level of sophistication, community based organizations may have a tougher time utilizing the tool with limited IT infrastructure than a large health system.”Regardless of the approach to organize data, successful organizations under P4P work diligently to create a culture of reporting where data is used to generate real-time change in order to continually improve, perform, and be rewarded by earning incentive payments. - Alignment of organizational strategy and reporting requirements
In the end, providers will only achieve long-term sustainability if they can successfully align all aspects of their organizational strategy to the collective reporting requirements of all-payer managed care organizations. Increasingly, the industry is witnessing more alignment and standardization of requirements across MCOs, various P4P programs, and state Medicaid programs. Quality measures tied to reporting are continually evaluated through a multi-stakeholder process to ensure they are staying up to date with changing clinical practices and retire measures where all realistic improvement has been achieved. With measures being rotated and retired, successful organizations will look at their data and other national reporting sets to focus transformational efforts where the most improvement is needed, while also doing everything possible to plan for success in the next release of updated requirements. Successful strategic organizations will incorporate more than a focus on just the outcomes; they will strive to utilize the best technological infrastructure, data analytics, population health tools, employee training, operational practices, and patient satisfaction practices they have at their disposal.
- Clearly defined processes, communication and accountability
COPE Health Solutions can help your organization evaluate your current readiness for performance based payments, maximizing use of of existing reporting infrastructure, and aligning financial incentives with quality-based programs. Our team has extensive experience in designing value based payment models driven by performance reporting and understand how to best improve your reporting practices if you are already participating in a pay-for-performance program. Additionally, our subject matter experts can help your system move toward its long-term strategic goals, using pilot programs such as Medicaid Waivers as a path to success.
For more information about how COPE Health Solutions is helping clients across the country prepare for value based payment and and improve reporting infrastructure, please contact: consulting@copy.laraco.net.