The Community Care Collaborative (CCC) in Travis County, Texas, demonstrates what can be accomplished through a Medicaid 1115 Waiver Delivery System Reform Incentive Payment (DSRIP) program. Under the program, the Collaborative expanded access to primary and specialty care, improved care for patients with chronic conditions, and integrated behavioral health care with primary care. Hitting these goals enabled the Collaborative to earn $49 million (100% of its available funds) in the second year of the DSRIP demonstration and $57 million (99.5% of its available funds) in the third year.
Inside the Waiver
The Centers for Medicaid and Medicare Services (CMS) approved Texas’ 1115 Medicaid Transformation Waiver in December 2011. Texas proposed the waiver to transform the delivery of health care to Medicaid and uninsured patient populations, as well as change how that care is paid for across the state. The state established 20 regional healthcare partnerships (RHP) that developed projects under the Delivery System Reform Incentive Payment (DSRIP) program. The DSRIP program enables participating providers to select five-year demonstration projects from a menu to transform care through infrastructure development, quality improvements, and redesigned health care delivery processes. Providers whose projects are approved receive incentive payments for successful implementation.
To participate in the waiver, Central Health, the healthcare district in Travis County that connects uninsured, underinsured, and low-income residents with high-quality, cost-effective health care, partnered with Seton Healthcare Family, a faith-based nonprofit health care system that operates more than 100 clinical locations, including four teaching hospitals—Dell Children’s Medical Center of Central Texas, University Medical Center Brackenridge, Seton Medical Center Austin, and Seton Shoal Creek Hospital, to form the CCC.
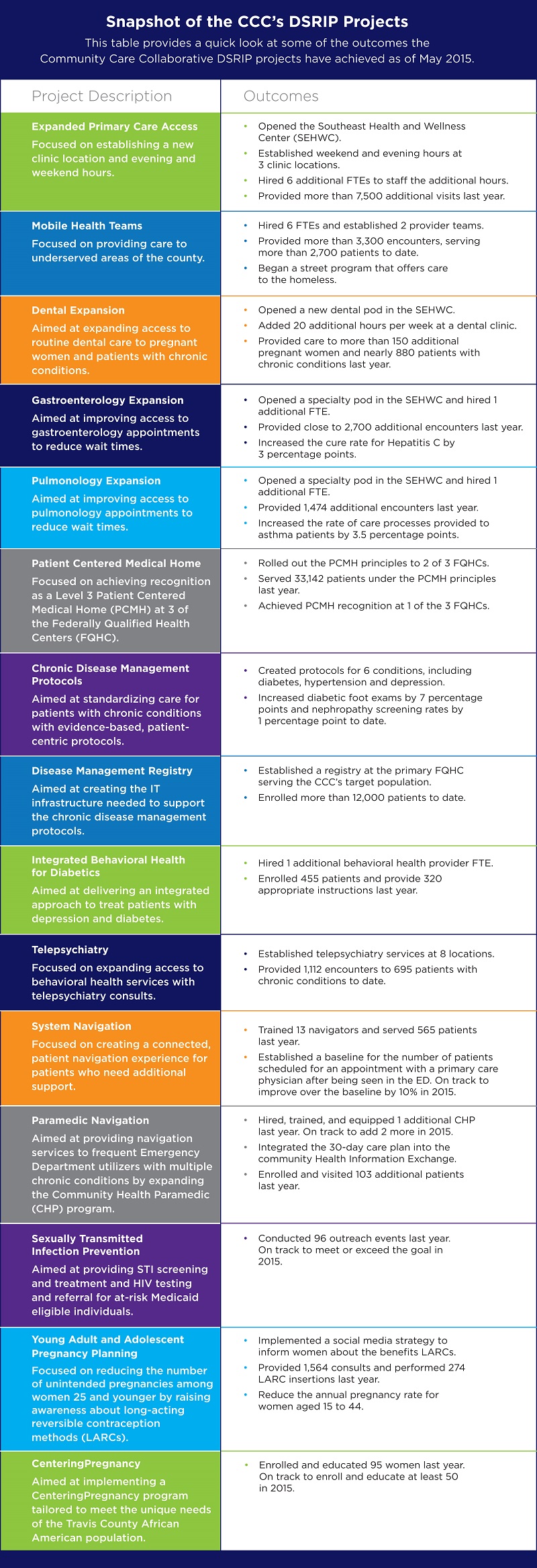
Recognizing that the CCC’s patient population grapples with chronic disease, behavioral-health related conditions, and health care access challenges, the CCC focused its 15 DSRIP projects to address those concerns. For example, to increase primary care availability and reduce specialty care waiting lists—which included one-year waits for visits to pulmonologists and gastroenterologists—the CCC increased primary care hours at certain sites to include evenings and weekends and added community-based specialty care. Other projects focused on developing critical infrastructure to support the CCC’s goal of providing an integrated delivery system for its safety-net patients. These infrastructure projects include launching disease management registry functionalities, developing a standardized approach for chronically ill patients, and promoting a neighborhood of patient-centered medical homes. The CCC designed and implemented the following 15 DSRIP projects:
- Expanded primary care access
- Mobile health provider teams
- Dental expansion
- Gastroenterology expansion
- Pulmonology expansion
- Patient-centered medical home
- Chronic disease management protocols
- Disease management registry
- Integrated behavioral health for diabetics
- Telepsychiatry
- System navigation
- Paramedic navigation
- Sexually transmitted infection prevention
- Young adult and adolescent pregnancy planning
- CenteringPregnancy program
Hitting Targeted Outcomes
The CCC monitors its projects and their effect on the patient population through a combination of (1) project milestones to track the progress of the DSRIP projects; (2) patient impact measures to quantify the patients impacted; and (3) quality metrics to quantify the impact on patients. The state uses these milestones, measures, and metrics to determine if the CCC qualifies for its incentive payments under the DSRIP program. Project milestones include opening a new primary care clinic, hiring clinicians to increase access, creating care protocols for chronic conditions, or training patient care navigators to help patients along the care continuum. Patient impact measures track the number of patients affected by a project or the number of encounters that the CCC is providing through a project. Quality metrics include the percentage of the diabetic population receiving annual screenings or the percentage of the hypertensive population whose blood pressure is controlled. (See the Snapshot of the CCC’s DSRIP Projects table for an expanded list of outcomes.)
Upon approval of the CCC DSRIP projects by the state, it became necessary to engage a third party to successfully achieve the CCC’s required measurement goals. The CCC hired COPE Health Solutions to develop implementation plans and help the CCC build its project management capabilities. Initially, COPE worked with all levels of the organization to determine the CCC’s needs and define the CCC’s goals. Next, COPE helped the CCC establish steering and workgroups comprised of stakeholders from Central Health, Seton, and the provider community to guide the implementation of the DSRIP projects. While the CCC worked on enhancing its community health information exchange capabilities, COPE set up a manual reporting structure that the CCC could begin using to track the milestones, measures, and metrics to show its progress. Together, the CCC and COPE Health Solutions achieved the change required to draw down 100% of its available funds in the second demonstration year and 99.5% of the funds available in the third year.
Lessons Learned
Currently in its fourth demonstration year, the state of Texas will likely file a renewal application in 2016 for its Medicaid 1115 Waiver program, which is expected to include a proposal to continue the DSRIP program beyond the initial five-year demonstration period. With another DSRIP program period on the horizon, and multiple other DSRIP-like programs developing in other states, here are five pieces of advice from the CCC’s experience with DSRIP:
- Define all aspects of health care provider partnership from the start. If you plan to partner with other health care organizations, discuss how you want to handle all aspects of the DSRIP programs early on. These aspects must include identification of financial, legal, and data-sharing risks and responsibilities. Otherwise, these critical operational details will require time and attention during the period better suited for program implementation.
- Examine what metrics would benefit your organization beyond the program requirements. Under the waiver program, providers must select their measures from a set menu. However, when you design your DSRIP projects, there may be other metrics that you should track to benefit your organization or patient population that are more effective measures than the program metrics. These should be built into programming at the outset of the project period to reduce unnecessary distractions later.
- Be prepared to implement changes that aren’t part of the DSRIP project intervention. Achieving quality improvements may require more than implementation of the intervention described in the DSRIP project. For example, one large FQHC working with the CCC to improve annual screenings realized that it made more sense to centralize its screening process rather than having providers do it themselves. It set up a referral center and patients that need multiple screenings are now contacted only once rather than receiving multiple calls. Although this change was not a required element of DSRIP, it had an immediate impact on the quality outcomes required by DSRIP.
- Think beyond the DSRIP demonstration period. Many providers in Texas, including the CCC, are starting to evaluate which projects are sustainable and should be continued after the DSRIP program ends. However, providers should evaluate which projects they would like continue at the beginning of the demonstration period. Aligning projects with strategy, planning for transition, and establishing a measurement and evaluation framework early in the process help ensure you get the most value out of your investment.
- Evaluate the impact of program implementation on care delivery. After the CCC removed bottlenecks in its specialty care process, it uncovered other issues that needed to be addressed. It is important to examine the entire delivery system to understand the impact of enhanced services in one area, including the alignment of funding for the impacted areas.
For more information on how COPE can help you succeed with DSRIP or other Medicaid redesign efforts in Texas or and other states contact: DSRIP@copy.laraco.net.
This table provides a quick look at some of the outcomes the Community Care Collaborative DSRIP projects have achieved as of May 2015.